Monday Poster Session
Category: Biliary/Pancreas
P1475 - Pseudomyxoma Peritonei from Spontaneous Rupture of a Recurrent Intraductal Papillary Mucinous Neoplasm After Total Pancreatectomy
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Mark Cromer, MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Mark Cromer, MD, Frederick Weber, MD
University of Alabama at Birmingham, Birmingham, AL
Introduction: Intraductal papillary mucinous neoplasms (IPMNs) are a common, premalignant form of pancreatic cystic neoplasm. Pseudomyxoma Peritonei (PMP) is a rare clinical syndrome characterized by diffuse peritoneal spread of a gelatinous mucinous material derived from an epithelial neoplasm, typically appendiceal or ovarian. PMP arising from a pancreatic IPMN is exceptionally rare and limited to a few case reports.
Case Description/Methods: A 58-year-old female with a history of hemorrhagic pancreatitis status post pancreatic debridement underwent distal pancreatectomy for tissue with high grade dysplasia (HGD). Four years post-operatively, surveillance abdominal CT scan found a new 1.2cm hypodensity of the pancreatic body. Subsequent endoscopic ultrasound (EUS) with fine needle aspiration (FNA) was consistent with a side branch IPMN with high-risk features. Resection of the pancreatic body was performed showing IPMN with HGD on pathology. Surveillance imaging later revealed near-complete replacement of the remnant pancreatic head with multilocular cystic lesions suggestive of recurrent multifocal IPMN. EUS with FNA again confirmed a side branch IPMN with high-risk features. Total pancreatectomy was then completed. Multi-institution review of the surgical pathology revealed extensive HGD without malignancy or lymphatic involvement. Three years later, surveillance imaging showed a new multi-cystic lesion in the prior pancreatic head region with multiple enlarged intra-abdominal lymph nodes, also confirmed by EUS. Weeks later she experienced acute RUQ pain, and subsequent MRCP highlighted new dense mucinous material along the liver periphery suggesting spontaneous cyst rupture and resultant PMP. Percutaneous biopsy of a perihepatic deposit confirmed a mucinous epithelial neoplasm consistent with PMP. The patient was ultimately referred for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy.
Discussion: Branch duct (BD) IPMNs carry an overall malignant potential of 20% at 10 years. Surgical resection is recommended for BD-IPMNs with multiple high-risk radiographic features for malignancy. Post-resection development of new IPMNs in residual pancreatic tissue may occur in up to 12.5% of cases. Peritoneal carcinomatosis arises from malignant metastatic peritoneal tumor deposits, whereas the mucin in PMP is often histologically benign. This case highlights the importance of IPMN and pancreatic remnant surveillance due to their risk of malignant conversion and IPMN recurrence, respectively.

Disclosures:
Mark Cromer, MD, Frederick Weber, MD. P1475 - Pseudomyxoma Peritonei from Spontaneous Rupture of a Recurrent Intraductal Papillary Mucinous Neoplasm After Total Pancreatectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Alabama at Birmingham, Birmingham, AL
Introduction: Intraductal papillary mucinous neoplasms (IPMNs) are a common, premalignant form of pancreatic cystic neoplasm. Pseudomyxoma Peritonei (PMP) is a rare clinical syndrome characterized by diffuse peritoneal spread of a gelatinous mucinous material derived from an epithelial neoplasm, typically appendiceal or ovarian. PMP arising from a pancreatic IPMN is exceptionally rare and limited to a few case reports.
Case Description/Methods: A 58-year-old female with a history of hemorrhagic pancreatitis status post pancreatic debridement underwent distal pancreatectomy for tissue with high grade dysplasia (HGD). Four years post-operatively, surveillance abdominal CT scan found a new 1.2cm hypodensity of the pancreatic body. Subsequent endoscopic ultrasound (EUS) with fine needle aspiration (FNA) was consistent with a side branch IPMN with high-risk features. Resection of the pancreatic body was performed showing IPMN with HGD on pathology. Surveillance imaging later revealed near-complete replacement of the remnant pancreatic head with multilocular cystic lesions suggestive of recurrent multifocal IPMN. EUS with FNA again confirmed a side branch IPMN with high-risk features. Total pancreatectomy was then completed. Multi-institution review of the surgical pathology revealed extensive HGD without malignancy or lymphatic involvement. Three years later, surveillance imaging showed a new multi-cystic lesion in the prior pancreatic head region with multiple enlarged intra-abdominal lymph nodes, also confirmed by EUS. Weeks later she experienced acute RUQ pain, and subsequent MRCP highlighted new dense mucinous material along the liver periphery suggesting spontaneous cyst rupture and resultant PMP. Percutaneous biopsy of a perihepatic deposit confirmed a mucinous epithelial neoplasm consistent with PMP. The patient was ultimately referred for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy.
Discussion: Branch duct (BD) IPMNs carry an overall malignant potential of 20% at 10 years. Surgical resection is recommended for BD-IPMNs with multiple high-risk radiographic features for malignancy. Post-resection development of new IPMNs in residual pancreatic tissue may occur in up to 12.5% of cases. Peritoneal carcinomatosis arises from malignant metastatic peritoneal tumor deposits, whereas the mucin in PMP is often histologically benign. This case highlights the importance of IPMN and pancreatic remnant surveillance due to their risk of malignant conversion and IPMN recurrence, respectively.

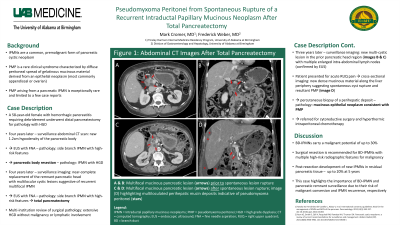
Figure: Figure 1: Abdominal CT scan images after total pancreatectomy.
A and B: Multifocal mucinous pancreatic lesion (arrows) prior to spontaneous lesion rupture; C and D: Multifocal mucinous pancreatic lesion (arrows) after spontaneous lesion rupture, with (D) highlighting multiloculated perihepatic mucin deposits indicative of pseudomyxoma peritonei (stars).
A and B: Multifocal mucinous pancreatic lesion (arrows) prior to spontaneous lesion rupture; C and D: Multifocal mucinous pancreatic lesion (arrows) after spontaneous lesion rupture, with (D) highlighting multiloculated perihepatic mucin deposits indicative of pseudomyxoma peritonei (stars).
Disclosures:
Mark Cromer indicated no relevant financial relationships.
Frederick Weber indicated no relevant financial relationships.
Mark Cromer, MD, Frederick Weber, MD. P1475 - Pseudomyxoma Peritonei from Spontaneous Rupture of a Recurrent Intraductal Papillary Mucinous Neoplasm After Total Pancreatectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
