Monday Poster Session
Category: Biliary/Pancreas
P1477 - Two for the Price of One: Concomitant Autoimmune Pancreatitis and Pancreatic Ductal Adenocarcinoma
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- CP
Chandler Patton, DO
Lehigh Valley Health Network
Allentown, PA
Presenting Author(s)
Chandler Patton, DO, Henry Lam, DO, Travis Magdaleno, DO, Hiral Shah, MD, Jeffrey Brodsky, MD
Lehigh Valley Health Network, Allentown, PA
Introduction: Autoimmune pancreatitis (AIP) is a rare, albeit significant cause of acute pancreatitis. It is characterized by unique findings, including responsiveness to steroid treatment. Radiographically, AIP can mimic pancreatic cancer, which often needs to be ruled out as part of the diagnostic evaluation. Here, we present a rare case of histologic concomitant AIP and pancreatic ductal adenocarcinoma (PDAC).
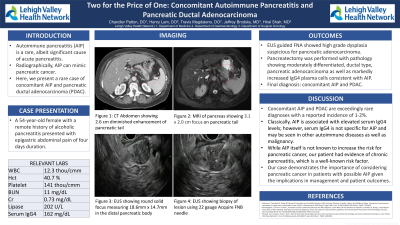
Case Description/Methods: A 54-year-old female with a remote history of alcoholic pancreatitis presented with epigastric abdominal pain of four days duration. Initial labs were significant for leukocytosis of 12.3 thou/cmm and mildly elevated lipase 202 U/L. CTAP showed peripancreatic edema with focal diminished enhancement of the distal pancreas. Follow-up MRI revealed a 3.1 x 2.0 cm focus in the pancreatic tail with peripancreatic lymphadenopathy concerning for pancreatitis versus malignancy. Additional workup revealed elevated serum IgG4 162 mg/dL suggesting possible AIP. Subsequently, the patient underwent further evaluation via EUS which showed pancreatic edema. Initial FNA sampling was nondiagnostic although chronic pancreatitis features were appreciated. Repeat sampling demonstrated atypical gland formation with high grade dysplasia suspicious for pancreatic adenocarcinoma. After surgical discussion, the patient underwent distal pancreatectomy. Pathology confirmed moderately differentiated, ductal type pancreatic adenocarcinoma. Interestingly, there was also lymphoplasmacytic chronic inflammation and associated sclerosing fibrosis with markedly increased IgG4 plasma cells consistent with AIP. The patient was ultimately diagnosed with concomitant AIP and PDAC. She was referred to oncology and initiated on adjuvant chemotherapy.
Discussion: Concomitant AIP and PDAC are exceedingly rare diagnoses with a reported incidence of 1-2%. Classically, AIP is associated with elevated serum IgG4 levels; however, serum IgG4 is not specific for AIP and may be seen in other autoimmune diseases as well as malignancy. While AIP itself is not known to increase the risk for pancreatic cancer, our patient had evidence of chronic pancreatitis, which is a well-known risk factor. The cause of her chronic pancreatitis is speculatory, but it is likely a culmination of significant tobacco and alcohol use with possible contribution by subclinical AIP. Our case demonstrates the importance of considering pancreatic cancer in patients with possible AIP given the implications in management and patient outcomes.
Disclosures:
Chandler Patton, DO, Henry Lam, DO, Travis Magdaleno, DO, Hiral Shah, MD, Jeffrey Brodsky, MD. P1477 - Two for the Price of One: Concomitant Autoimmune Pancreatitis and Pancreatic Ductal Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Lehigh Valley Health Network, Allentown, PA
Introduction: Autoimmune pancreatitis (AIP) is a rare, albeit significant cause of acute pancreatitis. It is characterized by unique findings, including responsiveness to steroid treatment. Radiographically, AIP can mimic pancreatic cancer, which often needs to be ruled out as part of the diagnostic evaluation. Here, we present a rare case of histologic concomitant AIP and pancreatic ductal adenocarcinoma (PDAC).
Case Description/Methods: A 54-year-old female with a remote history of alcoholic pancreatitis presented with epigastric abdominal pain of four days duration. Initial labs were significant for leukocytosis of 12.3 thou/cmm and mildly elevated lipase 202 U/L. CTAP showed peripancreatic edema with focal diminished enhancement of the distal pancreas. Follow-up MRI revealed a 3.1 x 2.0 cm focus in the pancreatic tail with peripancreatic lymphadenopathy concerning for pancreatitis versus malignancy. Additional workup revealed elevated serum IgG4 162 mg/dL suggesting possible AIP. Subsequently, the patient underwent further evaluation via EUS which showed pancreatic edema. Initial FNA sampling was nondiagnostic although chronic pancreatitis features were appreciated. Repeat sampling demonstrated atypical gland formation with high grade dysplasia suspicious for pancreatic adenocarcinoma. After surgical discussion, the patient underwent distal pancreatectomy. Pathology confirmed moderately differentiated, ductal type pancreatic adenocarcinoma. Interestingly, there was also lymphoplasmacytic chronic inflammation and associated sclerosing fibrosis with markedly increased IgG4 plasma cells consistent with AIP. The patient was ultimately diagnosed with concomitant AIP and PDAC. She was referred to oncology and initiated on adjuvant chemotherapy.
Discussion: Concomitant AIP and PDAC are exceedingly rare diagnoses with a reported incidence of 1-2%. Classically, AIP is associated with elevated serum IgG4 levels; however, serum IgG4 is not specific for AIP and may be seen in other autoimmune diseases as well as malignancy. While AIP itself is not known to increase the risk for pancreatic cancer, our patient had evidence of chronic pancreatitis, which is a well-known risk factor. The cause of her chronic pancreatitis is speculatory, but it is likely a culmination of significant tobacco and alcohol use with possible contribution by subclinical AIP. Our case demonstrates the importance of considering pancreatic cancer in patients with possible AIP given the implications in management and patient outcomes.
Disclosures:
Chandler Patton indicated no relevant financial relationships.
Henry Lam indicated no relevant financial relationships.
Travis Magdaleno indicated no relevant financial relationships.
Hiral Shah indicated no relevant financial relationships.
Jeffrey Brodsky indicated no relevant financial relationships.
Chandler Patton, DO, Henry Lam, DO, Travis Magdaleno, DO, Hiral Shah, MD, Jeffrey Brodsky, MD. P1477 - Two for the Price of One: Concomitant Autoimmune Pancreatitis and Pancreatic Ductal Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
