Monday Poster Session
Category: Biliary/Pancreas
P1481 - An Unusual Case of Abdominal Pain
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- SN
Srinivasan Narayanan
Southampton Medical Center
Southampton, England, United Kingdom
Presenting Author(s)
Srinivasan Narayanan, MBBS1, Pugazh Kandaswamy, MBBS, DCH, FRCPCH2, Natania Arun, 3, Shreya Naga. Ramachandran, 4, Balachandar Kathirvelu, MBBS, PhD5
1University Hospital Southampton, Southampton, England, United Kingdom; 2Aneurin Bevan University Health Board, Newport, Wales, United Kingdom; 3BASIS, Phoenix, AZ; 4Blue Valley North High School, Overland Park, KS; 5University of Texas, El Paso, El Paso, TX
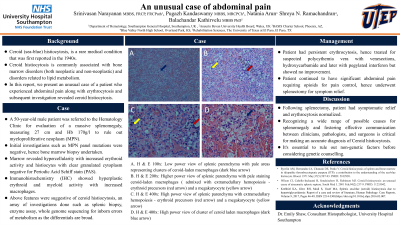
Introduction: Ceroid (sea-blue) histiocytosis, also known as sea-blue histiocytosis, is a rare medical condition that was first reported in the 1940s. Due to its infrequency, it is often overlooked or misdiagnosed. The condition mainly affects the spleen, bone marrow, and liver, although occurrences in other areas such as the skin and lungs have been reported. Ceroid histiocytosis is commonly associated with bone marrow disorders (both neoplastic and non-neoplastic) and disorders related to lipid metabolism. In this report, we present a case of a patient who experienced splenic pain, splenomegaly, erythrocytosis, and a subsequent biopsy revealed ceroid histiocytosis.
Case Description/Methods: A 50-year-old male patient was referred to the Hematology Clinic for evaluation of a massive splenomegaly, measuring 27 cm. Despite normal lab work, the patient was experiencing severe splenic pain and required opioids for pain control. A bone marrow biopsy was arranged due to suspicion of a myeloproliferative neoplasm, which revealed hypercellularity with increased erythroid activity and histiocytes with clear granulated cytoplasm negative for Periodic Acid Schiff stain (PAS). Immunohistochemistry (IHC) showed hyperplastic erythroid and myeloid activity with increased macrophages. The patient was initially treated for suspected polycythemia vera with hydroxycarbamide and later with pegylated interferon, but showed no improvement. Eventually, the patient underwent splenectomy for symptom relief. The microscopic examination revealed numerous macrophages/histiocytes with foamy cytoplasm, some containing small flecks of golden-brown pigments, possibly representing hemosiderin or lipofuscin. Significant extramedullary hematopoiesis within the spleen was noted, with numerous red blood cells and dilated sinusoids with relatively unstimulated white pulp activity. The hilar lymph node (LN) showed preserved architecture with sinus histiocytosis and scattered reactive follicles. IHC analysis showed normal distribution of B and T cells within the hilar LN and polytypic light chain expression. Despite the challenging diagnosis, the patient received appropriate care and support throughout their treatment and recovery.
Discussion: Recognizing a wide range of possible causes for splenomegaly and fostering effective communication between clinicians, pathologists, and surgeons is critical for making an accurate diagnosis in cases like this. It's essential to rule out non-genetic factors before considering genetic counselling.
Disclosures:
Srinivasan Narayanan, MBBS1, Pugazh Kandaswamy, MBBS, DCH, FRCPCH2, Natania Arun, 3, Shreya Naga. Ramachandran, 4, Balachandar Kathirvelu, MBBS, PhD5. P1481 - An Unusual Case of Abdominal Pain, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University Hospital Southampton, Southampton, England, United Kingdom; 2Aneurin Bevan University Health Board, Newport, Wales, United Kingdom; 3BASIS, Phoenix, AZ; 4Blue Valley North High School, Overland Park, KS; 5University of Texas, El Paso, El Paso, TX
Introduction: Ceroid (sea-blue) histiocytosis, also known as sea-blue histiocytosis, is a rare medical condition that was first reported in the 1940s. Due to its infrequency, it is often overlooked or misdiagnosed. The condition mainly affects the spleen, bone marrow, and liver, although occurrences in other areas such as the skin and lungs have been reported. Ceroid histiocytosis is commonly associated with bone marrow disorders (both neoplastic and non-neoplastic) and disorders related to lipid metabolism. In this report, we present a case of a patient who experienced splenic pain, splenomegaly, erythrocytosis, and a subsequent biopsy revealed ceroid histiocytosis.
Case Description/Methods: A 50-year-old male patient was referred to the Hematology Clinic for evaluation of a massive splenomegaly, measuring 27 cm. Despite normal lab work, the patient was experiencing severe splenic pain and required opioids for pain control. A bone marrow biopsy was arranged due to suspicion of a myeloproliferative neoplasm, which revealed hypercellularity with increased erythroid activity and histiocytes with clear granulated cytoplasm negative for Periodic Acid Schiff stain (PAS). Immunohistochemistry (IHC) showed hyperplastic erythroid and myeloid activity with increased macrophages. The patient was initially treated for suspected polycythemia vera with hydroxycarbamide and later with pegylated interferon, but showed no improvement. Eventually, the patient underwent splenectomy for symptom relief. The microscopic examination revealed numerous macrophages/histiocytes with foamy cytoplasm, some containing small flecks of golden-brown pigments, possibly representing hemosiderin or lipofuscin. Significant extramedullary hematopoiesis within the spleen was noted, with numerous red blood cells and dilated sinusoids with relatively unstimulated white pulp activity. The hilar lymph node (LN) showed preserved architecture with sinus histiocytosis and scattered reactive follicles. IHC analysis showed normal distribution of B and T cells within the hilar LN and polytypic light chain expression. Despite the challenging diagnosis, the patient received appropriate care and support throughout their treatment and recovery.
Discussion: Recognizing a wide range of possible causes for splenomegaly and fostering effective communication between clinicians, pathologists, and surgeons is critical for making an accurate diagnosis in cases like this. It's essential to rule out non-genetic factors before considering genetic counselling.
Disclosures:
Srinivasan Narayanan indicated no relevant financial relationships.
Pugazh Kandaswamy indicated no relevant financial relationships.
Natania Arun indicated no relevant financial relationships.
Shreya Ramachandran indicated no relevant financial relationships.
Balachandar Kathirvelu indicated no relevant financial relationships.
Srinivasan Narayanan, MBBS1, Pugazh Kandaswamy, MBBS, DCH, FRCPCH2, Natania Arun, 3, Shreya Naga. Ramachandran, 4, Balachandar Kathirvelu, MBBS, PhD5. P1481 - An Unusual Case of Abdominal Pain, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
