Monday Poster Session
Category: Biliary/Pancreas
P1487 - A Rare Phenomenon: Acute Cholecystitis Presenting as Acute Inferior STEMI
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- DS
Dipam Shah, MD
Inova Fairfax Medical Campus
Fairfax, VA
Presenting Author(s)
Award: Presidential Poster Award
Dipam Shah, MD1, Haider Ghumman, MPH2, Ussama Ghumman, MD3, Lawrence Istrail, MD4, Muhammad Hanafi, MD3
1Inova Fairfax Medical Campus, Fairfax, VA; 2University of Florida Morsani College of Medicine, Tampa, FL; 3Bayhealth Gastroenterology, Dover, DE; 4Inova Health System, Falls Church, VA
Introduction: Several non-cardiac conditions have been associated with ischemic ECG changes such as sepsis, renal failure, and shock. However, such changes have rarely been reported in gallbladder pathology. We present an unusual case of acute cholecystitis presenting with acute ST elevations in a territorial pattern on ECG.
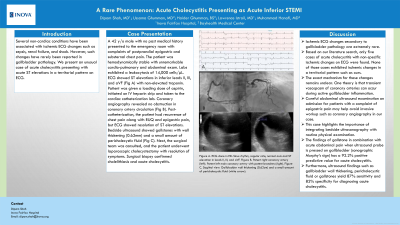
Case Description/Methods: A 42 y/o male with no past medical history presented to the emergency room with complaints of postprandial epigastric and substernal chest pain. The patient was hemodynamically stable with unremarkable cardio-pulmonary and abdominal exam. Labs exhibited a leukocytosis of 14,000 cells/μL. ECG showed ST elevations in inferior leads II, III, and aVF (Fig A) with non-elevated troponin. Patient was given a loading dose of aspirin, initiated on IV heparin drip and taken to the cardiac catheterization lab. Coronary angiography revealed no obstruction in coronary artery circulation (Fig B). Post-catheterization, the patient had recurrence of chest pain along with RUQ and epigastric pain, but ECG showed resolution of ST elevations. Bedside ultrasound showed gallstones with wall thickening (0.62mm) and a small amount of pericholecystic fluid (Fig C). Next, the surgical team was consulted, and the patient underwent laparoscopic cholecystectomy with resolution of symptoms. Surgical biopsy confirmed cholelithiasis and acute cholecystitis.
Discussion: Ischemic ECG changes secondary to gallbladder pathology are extremely rare. Based on our literature search, only five cases of acute cholecystitis with non-specific ischemic changes on ECG were found. None of those cases exhibited ischemic changes in a territorial pattern such as ours. The exact mechanism for these changes remains unclear. One theory is that transient vasospasm of coronary arteries can occur during active gallbladder inflammation. Careful abdominal ultrasound examination on admission for patients with a complaint of epigastric pain may help avoid invasive workup such as coronary angiography in our case. This case highlights the importance of integrating bedside ultrasonography with routine physical examination. The findings of gallstone in combination with acute abdominal pain when ultrasound probe is pressed on gallbladder (sonographic Murphy’s sign) has a 92.2% positive predictive value for acute cholecystitis. Furthermore, ultrasound findings such as gallbladder wall thickening, pericholecystic fluid or gallstones yield 87% sensitivity and 82% specificity for diagnosing acute cholecystitis.

Disclosures:
Dipam Shah, MD1, Haider Ghumman, MPH2, Ussama Ghumman, MD3, Lawrence Istrail, MD4, Muhammad Hanafi, MD3. P1487 - A Rare Phenomenon: Acute Cholecystitis Presenting as Acute Inferior STEMI, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Dipam Shah, MD1, Haider Ghumman, MPH2, Ussama Ghumman, MD3, Lawrence Istrail, MD4, Muhammad Hanafi, MD3
1Inova Fairfax Medical Campus, Fairfax, VA; 2University of Florida Morsani College of Medicine, Tampa, FL; 3Bayhealth Gastroenterology, Dover, DE; 4Inova Health System, Falls Church, VA
Introduction: Several non-cardiac conditions have been associated with ischemic ECG changes such as sepsis, renal failure, and shock. However, such changes have rarely been reported in gallbladder pathology. We present an unusual case of acute cholecystitis presenting with acute ST elevations in a territorial pattern on ECG.
Case Description/Methods: A 42 y/o male with no past medical history presented to the emergency room with complaints of postprandial epigastric and substernal chest pain. The patient was hemodynamically stable with unremarkable cardio-pulmonary and abdominal exam. Labs exhibited a leukocytosis of 14,000 cells/μL. ECG showed ST elevations in inferior leads II, III, and aVF (Fig A) with non-elevated troponin. Patient was given a loading dose of aspirin, initiated on IV heparin drip and taken to the cardiac catheterization lab. Coronary angiography revealed no obstruction in coronary artery circulation (Fig B). Post-catheterization, the patient had recurrence of chest pain along with RUQ and epigastric pain, but ECG showed resolution of ST elevations. Bedside ultrasound showed gallstones with wall thickening (0.62mm) and a small amount of pericholecystic fluid (Fig C). Next, the surgical team was consulted, and the patient underwent laparoscopic cholecystectomy with resolution of symptoms. Surgical biopsy confirmed cholelithiasis and acute cholecystitis.
Discussion: Ischemic ECG changes secondary to gallbladder pathology are extremely rare. Based on our literature search, only five cases of acute cholecystitis with non-specific ischemic changes on ECG were found. None of those cases exhibited ischemic changes in a territorial pattern such as ours. The exact mechanism for these changes remains unclear. One theory is that transient vasospasm of coronary arteries can occur during active gallbladder inflammation. Careful abdominal ultrasound examination on admission for patients with a complaint of epigastric pain may help avoid invasive workup such as coronary angiography in our case. This case highlights the importance of integrating bedside ultrasonography with routine physical examination. The findings of gallstone in combination with acute abdominal pain when ultrasound probe is pressed on gallbladder (sonographic Murphy’s sign) has a 92.2% positive predictive value for acute cholecystitis. Furthermore, ultrasound findings such as gallbladder wall thickening, pericholecystic fluid or gallstones yield 87% sensitivity and 82% specificity for diagnosing acute cholecystitis.

Figure: Figure A. ECG done in ED: Sinus rhythm, regular rate, normal axis and ST elevation in leads II, III, and aVF.
Figure B. Patent right coronary artery (left). Patent left main coronary artery with patent branches (right).
Figure C. Sagittal view: Gallbladder wall thickening (0.62cm) and a small amount of pericholecystic fluid (white arrow).
Figure B. Patent right coronary artery (left). Patent left main coronary artery with patent branches (right).
Figure C. Sagittal view: Gallbladder wall thickening (0.62cm) and a small amount of pericholecystic fluid (white arrow).
Disclosures:
Dipam Shah indicated no relevant financial relationships.
Haider Ghumman indicated no relevant financial relationships.
Ussama Ghumman indicated no relevant financial relationships.
Lawrence Istrail indicated no relevant financial relationships.
Muhammad Hanafi indicated no relevant financial relationships.
Dipam Shah, MD1, Haider Ghumman, MPH2, Ussama Ghumman, MD3, Lawrence Istrail, MD4, Muhammad Hanafi, MD3. P1487 - A Rare Phenomenon: Acute Cholecystitis Presenting as Acute Inferior STEMI, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

