Monday Poster Session
Category: Biliary/Pancreas
P1543 - When Considering the Rare Diagnosis of Lemmel's Syndrome, Be Sure to Leave No Stone Unturned
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- AM
Alexander Miller, MD
Guthrie Robert Packer Hospital
Sayre, Pennsylvania
Presenting Author(s)
Alexander Miller, MD, Michelle Bernshteyn, MD, Matthew Lincoln, DO
Guthrie Robert Packer Hospital, Sayre, PA
Introduction: When evaluating a patient with obstructive jaundice, a differential diagnosis inclusive of rare etiologies is important. However, it is essential to ensure that common causes continue to be considered during evaluation. Here, we present a patient with extrahepatic cholestasis and discuss his evaluation and management.
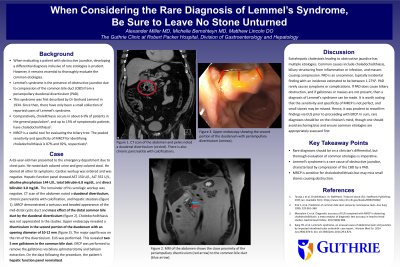
Case Description/Methods: A 65-year-old man presented to the emergency department due to chest pain. He noted dark colored urine and grey colored stool. He denied all other GI symptoms. Cardiac workup was ordered and was negative. Hepatic function panel showed AST 150 U/L, ALT 352 U/L, alkaline phosphatase 144 U/L, total bilirubin 6.8 mg/dL, and direct bilirubin 3.8 mg/dL. The remainder of his serologic workup was negative. CT scan of the abdomen noted a duodenal diverticulum, chronic pancreatitis with calcification, and hepatic steatosis. MRCP demonstrated a tortuous and beaded appearance of the mid-distal cystic duct and mass effect of the distal common bile duct by the duodenal diverticulum. Choledocholithiasis was not appreciated in the studies. Upper endoscopy revealed a diverticulum in the second portion of the duodenum with a mouth about 10-12 mm in diameter. The major papilla was on the rim of the diverticulum. EUS was performed. This revealed two 5 mm gallstones in the common bile duct. ERCP was performed to remove the gallstones via biliary sphincterotomy and balloon extraction. On the days following the procedure, the patient’s hepatic function panel normalized.
Discussion: Extrahepatic cholestasis leading to obstructive jaundice has multiple etiologies. Common causes include choledocholithiasis, biliary structuring from inflammation or infection, and masses causing compression. Periampullary duodenal diverticulum (PAD) is an uncommon, typically incidental finding with an incidence estimated to be between 1-27%. Of those with a PAD, about 5% will have complications such as obstruction, cholangitis, or acute pancreatitis. If PAD does cause biliary obstruction, and if gallstones or masses are not present, then a diagnosis of Lemmel’s syndrome can be made. It is worth noting that the sensitivity and accuracy of MRCP has been previously described as 90% and 89% respectively. Hence, it was prudent to reconfirm findings via EUS prior to proceeding with ERCP. In sum, rare diagnoses should be on the clinician’s mind, though one should avoid anchoring bias and ensure common etiologies are appropriately assessed first.

Disclosures:
Alexander Miller, MD, Michelle Bernshteyn, MD, Matthew Lincoln, DO. P1543 - When Considering the Rare Diagnosis of Lemmel's Syndrome, Be Sure to Leave No Stone Unturned, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Guthrie Robert Packer Hospital, Sayre, PA
Introduction: When evaluating a patient with obstructive jaundice, a differential diagnosis inclusive of rare etiologies is important. However, it is essential to ensure that common causes continue to be considered during evaluation. Here, we present a patient with extrahepatic cholestasis and discuss his evaluation and management.
Case Description/Methods: A 65-year-old man presented to the emergency department due to chest pain. He noted dark colored urine and grey colored stool. He denied all other GI symptoms. Cardiac workup was ordered and was negative. Hepatic function panel showed AST 150 U/L, ALT 352 U/L, alkaline phosphatase 144 U/L, total bilirubin 6.8 mg/dL, and direct bilirubin 3.8 mg/dL. The remainder of his serologic workup was negative. CT scan of the abdomen noted a duodenal diverticulum, chronic pancreatitis with calcification, and hepatic steatosis. MRCP demonstrated a tortuous and beaded appearance of the mid-distal cystic duct and mass effect of the distal common bile duct by the duodenal diverticulum. Choledocholithiasis was not appreciated in the studies. Upper endoscopy revealed a diverticulum in the second portion of the duodenum with a mouth about 10-12 mm in diameter. The major papilla was on the rim of the diverticulum. EUS was performed. This revealed two 5 mm gallstones in the common bile duct. ERCP was performed to remove the gallstones via biliary sphincterotomy and balloon extraction. On the days following the procedure, the patient’s hepatic function panel normalized.
Discussion: Extrahepatic cholestasis leading to obstructive jaundice has multiple etiologies. Common causes include choledocholithiasis, biliary structuring from inflammation or infection, and masses causing compression. Periampullary duodenal diverticulum (PAD) is an uncommon, typically incidental finding with an incidence estimated to be between 1-27%. Of those with a PAD, about 5% will have complications such as obstruction, cholangitis, or acute pancreatitis. If PAD does cause biliary obstruction, and if gallstones or masses are not present, then a diagnosis of Lemmel’s syndrome can be made. It is worth noting that the sensitivity and accuracy of MRCP has been previously described as 90% and 89% respectively. Hence, it was prudent to reconfirm findings via EUS prior to proceeding with ERCP. In sum, rare diagnoses should be on the clinician’s mind, though one should avoid anchoring bias and ensure common etiologies are appropriately assessed first.

Figure: Computed tomography (CT) scan of the abdomen and pelvis noted a duodenal diverticulum, chronic pancreatitis with calcification, and hepatic steatosis.
Disclosures:
Alexander Miller indicated no relevant financial relationships.
Michelle Bernshteyn indicated no relevant financial relationships.
Matthew Lincoln indicated no relevant financial relationships.
Alexander Miller, MD, Michelle Bernshteyn, MD, Matthew Lincoln, DO. P1543 - When Considering the Rare Diagnosis of Lemmel's Syndrome, Be Sure to Leave No Stone Unturned, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
