Monday Poster Session
Category: Biliary/Pancreas
P1547 - Undifferentiated Carcinoma of the Pancreas With Osteoclast-Like Giant Cells: A Grave Oncologic Diagnosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Clive J. Miranda, DO, MS
University at Buffalo
Buffalo, NY
Presenting Author(s)
Clive J. Miranda, DO, MS, Farhan Azad, DO, Alexander M. Carlson, DO, Eric J. Dove, MD, Muddasir Ayaz, MD
University at Buffalo, Buffalo, NY
Introduction: Undifferentiated carcinoma of the pancreas with osteoclast-like giant cells (UC-OGC) accounts for less than 1% of all pancreatic malignancies. It is typically diagnosed at advanced stages and frequently found to be unresectable. The prognosis is variable, depending on the presence of an associated pancreatic ductal adenocarcinoma (PDC).
Case Description/Methods: A 51-year-old male with no prior gastrointestinal (GI) history initially presented with complaints of recent 50lb weight loss, severe abdominal pain radiating to his back, vomiting, and an inability to tolerate solid food. He had a tender abdomen with a firm nodule palpated in the epigastrium. Bloodwork showed normal hemoglobin, white blood cells, platelets, and liver and kidney functionality. CA-19-9 (8 U/mL) and CEA (1.7 U/mL) were also normal. CT abdomen revealed fat stranding around the head of the pancreas (HOP), portal vein (PV) and superior mesenteric vein thrombosis, and peripancreatic adenopathy. There was a large mass in the third portion of the duodenum (D3) encasing branches of the superior mesenteric artery with gastric dilatation. Further evaluation via EGD/EUS showed a 67 x 60 mm fungating. villous mass with cystic components in D3 extending proximally to the stomach with intrinsic stenosis of the second portion of the duodenum (D2) (Figures 1-3). There was collateralization from the occluded PV around the HOP. The mass extended to the pancreas, but the pancreatic duct remained within normal limits. Biopsy via EUS showed undifferentiated carcinoma, with osteoclast-like giant cells, likely pancreatic or duodenal in origin (Figure 4). Tumor cells were negative for CK7 and CAM5.2 (markers typically seen in PDC) and positive for CD68 and vimentin (seen in OGC). Two weeks later, the patient was readmitted for deconditioning, upper GI bleeding, and worsening abdominal pain. A repeat EGD showed gastric outlet obstruction from the pancreatic tumor compressing on the duodenum. Given his worsening performance and nutritional status, two intraluminal duodenal stents were placed. Per the patient’s wishes, he was transitioned to hospice care and eventually passed.
Discussion: Pure UC-OGC, given negative PDC markers, typically shows better survival rates than UC-OGC with PDC. However, literature on UC-OGC is scarce and largely based on case reports. First-line treatment is surgical resection; however, optimal management lacks consensus. UC-OGC represents an exceedingly rare oncologic entity with the need for more evidence-based studies.

Disclosures:
Clive J. Miranda, DO, MS, Farhan Azad, DO, Alexander M. Carlson, DO, Eric J. Dove, MD, Muddasir Ayaz, MD. P1547 - Undifferentiated Carcinoma of the Pancreas With Osteoclast-Like Giant Cells: A Grave Oncologic Diagnosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University at Buffalo, Buffalo, NY
Introduction: Undifferentiated carcinoma of the pancreas with osteoclast-like giant cells (UC-OGC) accounts for less than 1% of all pancreatic malignancies. It is typically diagnosed at advanced stages and frequently found to be unresectable. The prognosis is variable, depending on the presence of an associated pancreatic ductal adenocarcinoma (PDC).
Case Description/Methods: A 51-year-old male with no prior gastrointestinal (GI) history initially presented with complaints of recent 50lb weight loss, severe abdominal pain radiating to his back, vomiting, and an inability to tolerate solid food. He had a tender abdomen with a firm nodule palpated in the epigastrium. Bloodwork showed normal hemoglobin, white blood cells, platelets, and liver and kidney functionality. CA-19-9 (8 U/mL) and CEA (1.7 U/mL) were also normal. CT abdomen revealed fat stranding around the head of the pancreas (HOP), portal vein (PV) and superior mesenteric vein thrombosis, and peripancreatic adenopathy. There was a large mass in the third portion of the duodenum (D3) encasing branches of the superior mesenteric artery with gastric dilatation. Further evaluation via EGD/EUS showed a 67 x 60 mm fungating. villous mass with cystic components in D3 extending proximally to the stomach with intrinsic stenosis of the second portion of the duodenum (D2) (Figures 1-3). There was collateralization from the occluded PV around the HOP. The mass extended to the pancreas, but the pancreatic duct remained within normal limits. Biopsy via EUS showed undifferentiated carcinoma, with osteoclast-like giant cells, likely pancreatic or duodenal in origin (Figure 4). Tumor cells were negative for CK7 and CAM5.2 (markers typically seen in PDC) and positive for CD68 and vimentin (seen in OGC). Two weeks later, the patient was readmitted for deconditioning, upper GI bleeding, and worsening abdominal pain. A repeat EGD showed gastric outlet obstruction from the pancreatic tumor compressing on the duodenum. Given his worsening performance and nutritional status, two intraluminal duodenal stents were placed. Per the patient’s wishes, he was transitioned to hospice care and eventually passed.
Discussion: Pure UC-OGC, given negative PDC markers, typically shows better survival rates than UC-OGC with PDC. However, literature on UC-OGC is scarce and largely based on case reports. First-line treatment is surgical resection; however, optimal management lacks consensus. UC-OGC represents an exceedingly rare oncologic entity with the need for more evidence-based studies.

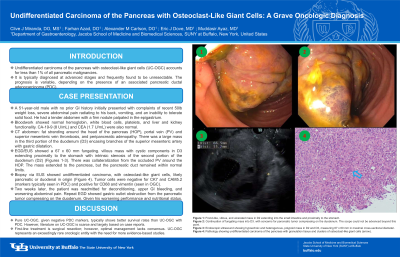
Figure: Figure 1: Frond-like, villous, and ulcerated mass in D2 extending into the small intestine and proximally to the stomach.
Figure 2: Continuation of fungating mass into D3. with concerns for pancreatic tumor compressing on the duodenum. The scope could not be advanced beyond this point.
Figure 3: Endoscopic ultrasound showing hypoechoic and heterogenous, polypoid mass in D2 and D3, measuring 67 x 60 mm in maximal cross-sectional diameter.
Figure 4: Pathology showing undifferentiated carcinoma of the pancreas with granulation tissue and clusters of osteoclast-like giant cells (arrow).
Figure 2: Continuation of fungating mass into D3. with concerns for pancreatic tumor compressing on the duodenum. The scope could not be advanced beyond this point.
Figure 3: Endoscopic ultrasound showing hypoechoic and heterogenous, polypoid mass in D2 and D3, measuring 67 x 60 mm in maximal cross-sectional diameter.
Figure 4: Pathology showing undifferentiated carcinoma of the pancreas with granulation tissue and clusters of osteoclast-like giant cells (arrow).
Disclosures:
Clive Miranda indicated no relevant financial relationships.
Farhan Azad indicated no relevant financial relationships.
Alexander Carlson indicated no relevant financial relationships.
Eric Dove indicated no relevant financial relationships.
Muddasir Ayaz indicated no relevant financial relationships.
Clive J. Miranda, DO, MS, Farhan Azad, DO, Alexander M. Carlson, DO, Eric J. Dove, MD, Muddasir Ayaz, MD. P1547 - Undifferentiated Carcinoma of the Pancreas With Osteoclast-Like Giant Cells: A Grave Oncologic Diagnosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
