Monday Poster Session
Category: Biliary/Pancreas
P1548 - Fetus and Maternal Outcomes in Primary Sclerosing Cholangitis With Choledocholithiasis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Karan B. Singh, MD
University of South Alabama
Mobile, AL
Presenting Author(s)
Karan B. Singh, MD, Chad Spencer, MD, Rajab Idriss, MD
University of South Alabama, Mobile, AL
Introduction: Chronic cholestatic liver diseases such as primary sclerosing cholangitis (PSC), primary biliary cholangitis (PBC), and intrahepatic cholestasis of pregnancy increase the risk of harm to the fetus due to immature blood-brain-barrier in fetuses. Chronic cholestatic disorders increase risk of gallstones, especially in pregnancy; management of choledocholithiasis in pregnancy is ERCP. We present a complex case of primary sclerosing cholangitis with recurrent choledocholithiasis and biliary structures requiring non-elective ERCP during the second trimester of pregnancy.
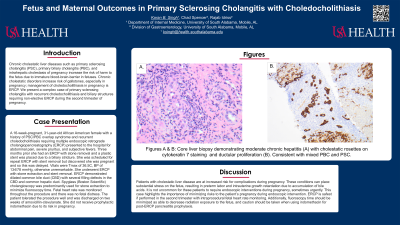
Case Description/Methods: A 16-week-pregnant, 31-year-old African American female with a history of PSC/PBC overlap syndrome and recurrent choledocholithiasis requiring multiple endoscopic retrograde cholangiopancreatography (ERCP) presented to the hospital for abdominal pain, severe pruritus, and subjective fevers. Three months prior she had an ERCP with stone removal and a plastic stent was placed due to a biliary stricture. She was scheduled for repeat ERCP with stent removal but discovered she was pregnant and so this was delayed. Vitals were Tmax of 36.5C, BP of 134/78 mmHg, otherwise unremarkable. She underwent ERCP with stone extraction and stent removal. ERCP demonstrated dilated common bile duct (CBD) with several filling defects in the CBD and common hepatic duct. Spyglass (Boston Scientific) cholangioscopy was predominantly used for stone extraction to minimize fluoroscopy time. Fetal heart rate was monitored throughout the procedure and there was no fetal distress. The patient tolerated the procedure well and was discharged on two weeks of amoxicillin-clavulanate. She did not receive prophylactic indomethacin due to its risk in pregnancy.
Discussion: Patients with cholestatic liver disease are at increased risk for complications during pregnancy. These conditions can place substantial stress on the fetus, resulting in preterm labor and intrauterine growth retardation due to accumulation of bile acids. It is not uncommon for these patients to require endoscopic interventions during pregnancy, sometimes urgently. This case highlights the importance of minimizing risks to the patient’s pregnancy during endoscopic intervention. ERCP is safest if performed in the second trimester with intraprocedural fetal heart rate monitoring. Additionally, fluoroscopy time should be minimized as able to decrease radiation exposure to the fetus, and caution should be taken when using indomethacin for post-ERCP pancreatitis prophylaxis.
Disclosures:
Karan B. Singh, MD, Chad Spencer, MD, Rajab Idriss, MD. P1548 - Fetus and Maternal Outcomes in Primary Sclerosing Cholangitis With Choledocholithiasis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of South Alabama, Mobile, AL
Introduction: Chronic cholestatic liver diseases such as primary sclerosing cholangitis (PSC), primary biliary cholangitis (PBC), and intrahepatic cholestasis of pregnancy increase the risk of harm to the fetus due to immature blood-brain-barrier in fetuses. Chronic cholestatic disorders increase risk of gallstones, especially in pregnancy; management of choledocholithiasis in pregnancy is ERCP. We present a complex case of primary sclerosing cholangitis with recurrent choledocholithiasis and biliary structures requiring non-elective ERCP during the second trimester of pregnancy.
Case Description/Methods: A 16-week-pregnant, 31-year-old African American female with a history of PSC/PBC overlap syndrome and recurrent choledocholithiasis requiring multiple endoscopic retrograde cholangiopancreatography (ERCP) presented to the hospital for abdominal pain, severe pruritus, and subjective fevers. Three months prior she had an ERCP with stone removal and a plastic stent was placed due to a biliary stricture. She was scheduled for repeat ERCP with stent removal but discovered she was pregnant and so this was delayed. Vitals were Tmax of 36.5C, BP of 134/78 mmHg, otherwise unremarkable. She underwent ERCP with stone extraction and stent removal. ERCP demonstrated dilated common bile duct (CBD) with several filling defects in the CBD and common hepatic duct. Spyglass (Boston Scientific) cholangioscopy was predominantly used for stone extraction to minimize fluoroscopy time. Fetal heart rate was monitored throughout the procedure and there was no fetal distress. The patient tolerated the procedure well and was discharged on two weeks of amoxicillin-clavulanate. She did not receive prophylactic indomethacin due to its risk in pregnancy.
Discussion: Patients with cholestatic liver disease are at increased risk for complications during pregnancy. These conditions can place substantial stress on the fetus, resulting in preterm labor and intrauterine growth retardation due to accumulation of bile acids. It is not uncommon for these patients to require endoscopic interventions during pregnancy, sometimes urgently. This case highlights the importance of minimizing risks to the patient’s pregnancy during endoscopic intervention. ERCP is safest if performed in the second trimester with intraprocedural fetal heart rate monitoring. Additionally, fluoroscopy time should be minimized as able to decrease radiation exposure to the fetus, and caution should be taken when using indomethacin for post-ERCP pancreatitis prophylaxis.
Disclosures:
Karan Singh indicated no relevant financial relationships.
Chad Spencer indicated no relevant financial relationships.
Rajab Idriss indicated no relevant financial relationships.
Karan B. Singh, MD, Chad Spencer, MD, Rajab Idriss, MD. P1548 - Fetus and Maternal Outcomes in Primary Sclerosing Cholangitis With Choledocholithiasis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
