Monday Poster Session
Category: Biliary/Pancreas
P1554 - An Unusual Case of Obstructive Jaundice
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Andrew Krane, MD
Warren Alpert Medical School of Brown University
Providence, RI
Presenting Author(s)
Andrew Krane, MD1, Naveena Sunkara, MD2, Boris Sinayuk, MD3, Jim ChunHao. Lee, MD, MPH4, Samir A. Shah, MD, FACG5
1Warren Alpert Medical School of Brown University, Providence, RI; 2Warren Alpert Medical School, Brown University, Providence, RI; 3Rhode Island Medical Imaging, Sharon, MA; 4Rhode Island Hospital, Providence, RI; 5Gastroenterology Associates, Inc., Providence, RI
Introduction: Malignant obstructive jaundice is caused by blockage or narrowing of the bile or pancreatic ducts, often due to cholangiocarcinoma, gallbladder or pancreatic carcinoma, or metastatic lymphadenopathy. Endoscopic retrograde cholangiopancreatography (ERCP) with stent placement or percutaneous transhepatic cholangiography and biliary drainage (PTCD) are commonly performed for relieving obstruction, but stent occlusion rates are high, requiring repeated procedures for palliation. Here we describe a rare etiology of obstructive jaundice from metastatic renal cell carcinoma (RCC).
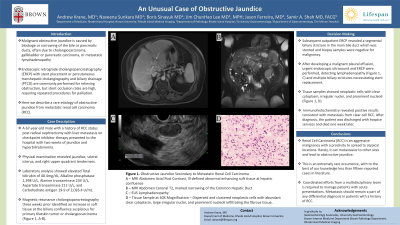
Case Description/Methods: A 67-year-old male with a history of RCC status post radical nephrectomy with liver metastasis on checkpoint inhibitor therapy presented to the hospital with two weeks of jaundice and hyperbilirubinemia. Physical examination revealed jaundice, scleral icterus, and right upper quadrant tenderness. Laboratory analysis showed elevated Total bilirubin of 40.4mg/dL, Alkaline phosphatase 1,398 U/L, Alanine transaminase 234 U/L, Aspartate transaminase 211 U/L, and Carbohydrate antigen 19-9 of 2,026.4 U/mL. Magnetic resonance cholangiopancreatography three weeks prior identified an increase in soft tissue at the biliary confluence suspicious for primary Klatskin tumor or cholangiocarcinoma (Figure 1, A-B). Subsequent outpatient ERCP revealed a segmental biliary stricture in the main bile duct which was stented and biopsy samples were negative for malignancy. This was repeated again during admission with further negative biopsy samples. After developing a malignant pleural effusion, urgent endoscopic ultrasound and ERCP were performed, detecting lymphadenopathy (Figure 1, C) and multiple biliary strictures necessitating stent replacement. Tissue samples showed neoplastic cells with clear cytoplasm, irregular nuclei, and prominent nucleoli (Figure 1, D). Immunohistochemistry revealed positive results consistent with metastasis from clear cell RCC. After diagnosis, the patient was discharged with hospice services and died one week later.
Discussion: Renal Cell Carcinoma (RCC) is an aggressive malignancy with a proclivity to spread to atypical locations, but more frequently to bone, lungs or lymph nodes. Rarely, it can metastasize to other sites and lead to obstructive jaundice. This is an extremely rare occurrence, with to the best of our knowledge less than fifteen reported cases in literature. Coordinated efforts from a multidisciplinary team is required to manage patients with acute presentations.

Disclosures:
Andrew Krane, MD1, Naveena Sunkara, MD2, Boris Sinayuk, MD3, Jim ChunHao. Lee, MD, MPH4, Samir A. Shah, MD, FACG5. P1554 - An Unusual Case of Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Warren Alpert Medical School of Brown University, Providence, RI; 2Warren Alpert Medical School, Brown University, Providence, RI; 3Rhode Island Medical Imaging, Sharon, MA; 4Rhode Island Hospital, Providence, RI; 5Gastroenterology Associates, Inc., Providence, RI
Introduction: Malignant obstructive jaundice is caused by blockage or narrowing of the bile or pancreatic ducts, often due to cholangiocarcinoma, gallbladder or pancreatic carcinoma, or metastatic lymphadenopathy. Endoscopic retrograde cholangiopancreatography (ERCP) with stent placement or percutaneous transhepatic cholangiography and biliary drainage (PTCD) are commonly performed for relieving obstruction, but stent occlusion rates are high, requiring repeated procedures for palliation. Here we describe a rare etiology of obstructive jaundice from metastatic renal cell carcinoma (RCC).
Case Description/Methods: A 67-year-old male with a history of RCC status post radical nephrectomy with liver metastasis on checkpoint inhibitor therapy presented to the hospital with two weeks of jaundice and hyperbilirubinemia. Physical examination revealed jaundice, scleral icterus, and right upper quadrant tenderness. Laboratory analysis showed elevated Total bilirubin of 40.4mg/dL, Alkaline phosphatase 1,398 U/L, Alanine transaminase 234 U/L, Aspartate transaminase 211 U/L, and Carbohydrate antigen 19-9 of 2,026.4 U/mL. Magnetic resonance cholangiopancreatography three weeks prior identified an increase in soft tissue at the biliary confluence suspicious for primary Klatskin tumor or cholangiocarcinoma (Figure 1, A-B). Subsequent outpatient ERCP revealed a segmental biliary stricture in the main bile duct which was stented and biopsy samples were negative for malignancy. This was repeated again during admission with further negative biopsy samples. After developing a malignant pleural effusion, urgent endoscopic ultrasound and ERCP were performed, detecting lymphadenopathy (Figure 1, C) and multiple biliary strictures necessitating stent replacement. Tissue samples showed neoplastic cells with clear cytoplasm, irregular nuclei, and prominent nucleoli (Figure 1, D). Immunohistochemistry revealed positive results consistent with metastasis from clear cell RCC. After diagnosis, the patient was discharged with hospice services and died one week later.
Discussion: Renal Cell Carcinoma (RCC) is an aggressive malignancy with a proclivity to spread to atypical locations, but more frequently to bone, lungs or lymph nodes. Rarely, it can metastasize to other sites and lead to obstructive jaundice. This is an extremely rare occurrence, with to the best of our knowledge less than fifteen reported cases in literature. Coordinated efforts from a multidisciplinary team is required to manage patients with acute presentations.

Figure: Figure 1: Obstructive Jaundice secondary to metastatic Renal Cell Carcinoma
A – MRI Abdomen Axial Post Contrast, Ill-defined abnormal enhancing soft tissue at hepatic confluence
B – MRI Abdomen Coronal T2, marked narrowing of the Common Hepatic Duct
C – EUS Lymphadenopathy
D – Tissue Sample at 40X Magnification – Dispersed and clustered neoplastic cells with abundant clear cytoplasm, large irregular nuclei, and prominent nucleoli infiltrating the fibrous tissue.
A – MRI Abdomen Axial Post Contrast, Ill-defined abnormal enhancing soft tissue at hepatic confluence
B – MRI Abdomen Coronal T2, marked narrowing of the Common Hepatic Duct
C – EUS Lymphadenopathy
D – Tissue Sample at 40X Magnification – Dispersed and clustered neoplastic cells with abundant clear cytoplasm, large irregular nuclei, and prominent nucleoli infiltrating the fibrous tissue.
Disclosures:
Andrew Krane indicated no relevant financial relationships.
Naveena Sunkara indicated no relevant financial relationships.
Boris Sinayuk indicated no relevant financial relationships.
Jim Lee indicated no relevant financial relationships.
Samir Shah indicated no relevant financial relationships.
Andrew Krane, MD1, Naveena Sunkara, MD2, Boris Sinayuk, MD3, Jim ChunHao. Lee, MD, MPH4, Samir A. Shah, MD, FACG5. P1554 - An Unusual Case of Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
