Monday Poster Session
Category: Biliary/Pancreas
P1569 - Type IV Paraesophageal Hernia Causing Pancreatitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sarah Grebennikov, DO, MHS
Riverside Methodist Hospital
Columbus, OH
Presenting Author(s)
Sarah Grebennikov, DO, MHS1, Jay Anderson, DO1, David Y. Lo, MD, FACG2
1Riverside Methodist Hospital, Columbus, OH; 2Ohio Gastroenterology Group, Inc., Columbus, OH
Introduction: A hiatal hernia (HH) occurs when a portion of the stomach protrudes through the esophageal hiatus. Most cases are asymptomatic; in rare cases, herniation of pancreas can occur which can lead to pancreatitis. We present a case of a type IV paraesophageal hernia (PEH) with inclusion of the pancreatic body and tail causing acute pancreatitis.
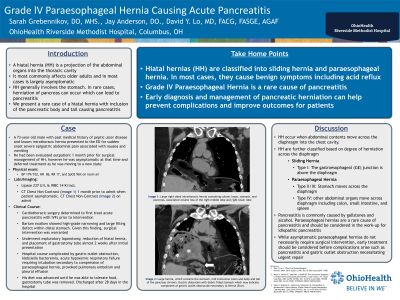
Case Description/Methods: 73-year-old male with past medical history of peptic ulcer disease and known intrathoracic hernia presented to the hospital with sudden onset epigastric abdominal pain, nausea, and vomiting. Labs were remarkable for lipase 237 U/L (normal < 65 U/L) and WBC 14 K/mcL. Liver function tests, calcium and triglyceride levels were normal. Computed tomography showed a large right PEH with a debris-filled stomach consistent with gastric outlet obstruction (asterisk). In addition, it contained the mid transverse colon, along with the body and tail of the pancreas (arrow). Cardiothoracic surgery initially pursued conservative management given active pancreatitis and gastric outlet obstruction. After resolution of pancreatitis and obstruction, the patient then underwent exploratory laparotomy, reduction of hiatal hernia, and placement of gastrostomy tube. One month later he was discharged tolerating a regular diet.
Discussion: HH are classified into four subtypes based on the location and size. The most severe form of HH is type IV PEH and occurs when other intraabdominal organs project into the thoracic cavity. The exact etiology is variable and can be congenital, smoking, age, and obesity. Clinical presentation can vary from asymptomatic, gastric reflux, to more severe complications such as obstruction from gastric volvulus, bleeding, and perforation. Pancreatitis is a rare complication of PEH and is thought to be caused by repetitive trauma, vascular insufficiency and pancreatic ductal obstruction. Diagnosis is based on imaging. Treatment options depend on the degree and severity of herniation. While asymptomatic paraesophageal hernias do not necessarily require surgical intervention, early treatment should be considered before complications arise.

Disclosures:
Sarah Grebennikov, DO, MHS1, Jay Anderson, DO1, David Y. Lo, MD, FACG2. P1569 - Type IV Paraesophageal Hernia Causing Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Riverside Methodist Hospital, Columbus, OH; 2Ohio Gastroenterology Group, Inc., Columbus, OH
Introduction: A hiatal hernia (HH) occurs when a portion of the stomach protrudes through the esophageal hiatus. Most cases are asymptomatic; in rare cases, herniation of pancreas can occur which can lead to pancreatitis. We present a case of a type IV paraesophageal hernia (PEH) with inclusion of the pancreatic body and tail causing acute pancreatitis.
Case Description/Methods: 73-year-old male with past medical history of peptic ulcer disease and known intrathoracic hernia presented to the hospital with sudden onset epigastric abdominal pain, nausea, and vomiting. Labs were remarkable for lipase 237 U/L (normal < 65 U/L) and WBC 14 K/mcL. Liver function tests, calcium and triglyceride levels were normal. Computed tomography showed a large right PEH with a debris-filled stomach consistent with gastric outlet obstruction (asterisk). In addition, it contained the mid transverse colon, along with the body and tail of the pancreas (arrow). Cardiothoracic surgery initially pursued conservative management given active pancreatitis and gastric outlet obstruction. After resolution of pancreatitis and obstruction, the patient then underwent exploratory laparotomy, reduction of hiatal hernia, and placement of gastrostomy tube. One month later he was discharged tolerating a regular diet.
Discussion: HH are classified into four subtypes based on the location and size. The most severe form of HH is type IV PEH and occurs when other intraabdominal organs project into the thoracic cavity. The exact etiology is variable and can be congenital, smoking, age, and obesity. Clinical presentation can vary from asymptomatic, gastric reflux, to more severe complications such as obstruction from gastric volvulus, bleeding, and perforation. Pancreatitis is a rare complication of PEH and is thought to be caused by repetitive trauma, vascular insufficiency and pancreatic ductal obstruction. Diagnosis is based on imaging. Treatment options depend on the degree and severity of herniation. While asymptomatic paraesophageal hernias do not necessarily require surgical intervention, early treatment should be considered before complications arise.

Figure: Computed tomography chest without IV contrast showed a large right paraesophageal hernia containing the mid transverse colon, body and tail of the pancreas (arrow), and a debris-filled stomach consistent with gastric outlet obstruction (asterisk).
Disclosures:
Sarah Grebennikov indicated no relevant financial relationships.
Jay Anderson indicated no relevant financial relationships.
David Lo indicated no relevant financial relationships.
Sarah Grebennikov, DO, MHS1, Jay Anderson, DO1, David Y. Lo, MD, FACG2. P1569 - Type IV Paraesophageal Hernia Causing Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
