Monday Poster Session
Category: Biliary/Pancreas
P1571 - A Rare Presentation of Gout
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Minh Do, MD
CU Internal Medicine Residency Program
Aurora, CO
Presenting Author(s)
Minh Do, MD1, Sridevi K. Pokala, MD2, Augustin R. Attwell, MD3
1CU Internal Medicine Residency Program, Aurora, CO; 2University of Colorado, Denver, CO; 3University of Colorado Medical School, Aurora, CO
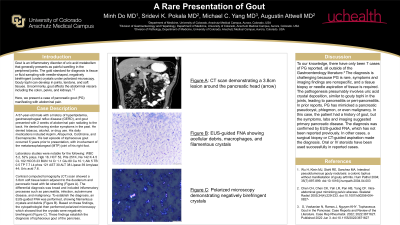
Introduction: Gout is an inflammatory disorder of uric acid metabolism that commonly presents as painful swelling of peripheral joints. Polarized microscopy of fluid obtained via arthrocentesis of involved joints classically shows needle-shaped, negatively birefringent crystals. Occasionally, gout affects the abdominal viscera including the colon, pelvis, and kidneys. Herein we describe a patient with abdominal pain due to pancreatic gout (PG).
Case Description/Methods: A 57-year-old male with a history of hyperlipidemia and gout presented with a 2-week history of abdominal pain radiating to the back. Laboratory studies were unremarkable, including complete metabolic panel, complete blood count, amylase, and lipase. Contrast computed tomography (CT) scan showed a 3.8cm soft tissue lesion around the duodenum and pancreatic head with adjacent fat stranding (A). Endoscopic ultrasound (EUS) revealed an ill-defined lesion in the peripancreatic region, including a 16.7mm by 9mm portion next to the pancreatic head. The duodenum, ampulla, and pancreatic head were normal. Fine-needle aspiration (FNA) of the lesion showed acellular debris, macrophages, and filamentous crystals that were negatively birefringent under polarized microscopy, confirming the diagnosis of PG (B). Steroids were considered but ultimately deferred since the patient’s symptoms improved spontaneously and resolved after 4 weeks. Follow-up magnetic resonance imaging (MRI) 6 weeks after EUS demonstrated near-resolution of the previous abnormalities (C).
Discussion: To our knowledge, there have only been 7 cases of PG reported, all from the Rheumatology literature. The diagnosis of PG is challenging because it is a rare disease, symptoms and imaging findings are nonspecific, and tissue biopsy or needle aspiration is required. PG may mimic a pseudocyst, phlegmon, or malignancy. Our patient had a prior diagnosis of gout, but the history, labs and imaging suggested pancreatic disease. The diagnosis of PG in this patient was established by EUS-guided FNA, which has not been reported previously. Surgical biopsy or CT-guided aspiration made the diagnoses in previously reported PG cases. Surveillance imaging further excluded malignancy in this patient. Although this patient did not require anti-inflammatory medications as his PG resolved spontaneously, successful use of oral or IV steroids has been reported in other cases. This case highlights the importance of considering PG for patients with gout who present with unexplained or atypical pancreatic lesions.

Disclosures:
Minh Do, MD1, Sridevi K. Pokala, MD2, Augustin R. Attwell, MD3. P1571 - A Rare Presentation of Gout, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1CU Internal Medicine Residency Program, Aurora, CO; 2University of Colorado, Denver, CO; 3University of Colorado Medical School, Aurora, CO
Introduction: Gout is an inflammatory disorder of uric acid metabolism that commonly presents as painful swelling of peripheral joints. Polarized microscopy of fluid obtained via arthrocentesis of involved joints classically shows needle-shaped, negatively birefringent crystals. Occasionally, gout affects the abdominal viscera including the colon, pelvis, and kidneys. Herein we describe a patient with abdominal pain due to pancreatic gout (PG).
Case Description/Methods: A 57-year-old male with a history of hyperlipidemia and gout presented with a 2-week history of abdominal pain radiating to the back. Laboratory studies were unremarkable, including complete metabolic panel, complete blood count, amylase, and lipase. Contrast computed tomography (CT) scan showed a 3.8cm soft tissue lesion around the duodenum and pancreatic head with adjacent fat stranding (A). Endoscopic ultrasound (EUS) revealed an ill-defined lesion in the peripancreatic region, including a 16.7mm by 9mm portion next to the pancreatic head. The duodenum, ampulla, and pancreatic head were normal. Fine-needle aspiration (FNA) of the lesion showed acellular debris, macrophages, and filamentous crystals that were negatively birefringent under polarized microscopy, confirming the diagnosis of PG (B). Steroids were considered but ultimately deferred since the patient’s symptoms improved spontaneously and resolved after 4 weeks. Follow-up magnetic resonance imaging (MRI) 6 weeks after EUS demonstrated near-resolution of the previous abnormalities (C).
Discussion: To our knowledge, there have only been 7 cases of PG reported, all from the Rheumatology literature. The diagnosis of PG is challenging because it is a rare disease, symptoms and imaging findings are nonspecific, and tissue biopsy or needle aspiration is required. PG may mimic a pseudocyst, phlegmon, or malignancy. Our patient had a prior diagnosis of gout, but the history, labs and imaging suggested pancreatic disease. The diagnosis of PG in this patient was established by EUS-guided FNA, which has not been reported previously. Surgical biopsy or CT-guided aspiration made the diagnoses in previously reported PG cases. Surveillance imaging further excluded malignancy in this patient. Although this patient did not require anti-inflammatory medications as his PG resolved spontaneously, successful use of oral or IV steroids has been reported in other cases. This case highlights the importance of considering PG for patients with gout who present with unexplained or atypical pancreatic lesions.

Figure: A. CT scan demonstrating a 3.8cm lesion around the pancreatic head (arrow)
B. Negatively birefringent crystals under polarized microscopy
C. Follow-up MRI demonstrating marked improvement in the lesion (arrow)
B. Negatively birefringent crystals under polarized microscopy
C. Follow-up MRI demonstrating marked improvement in the lesion (arrow)
Disclosures:
Minh Do indicated no relevant financial relationships.
Sridevi Pokala indicated no relevant financial relationships.
Augustin Attwell indicated no relevant financial relationships.
Minh Do, MD1, Sridevi K. Pokala, MD2, Augustin R. Attwell, MD3. P1571 - A Rare Presentation of Gout, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
