Monday Poster Session
Category: Colon
P1584 - Genetic Risk for Colorectal Cancer Is Associated With Earlier Onset and Higher Incidence of Immune Checkpoint Inhibitor Colitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- SG
Shilpa Grover, MD, MPH
Brigham and Women's Hospital
Boston, Massachusetts
Presenting Author(s)
Sarah Abou Alaiwi, MD1, Stefan Groha, PhD2, Sanchit Gupta, MD, MS1, Pier Vitale Nuzzo, MD, PhD3, Amin Nassar, MD1, Talal El Zarif, MD2, Elio Adib, MD2, Jordan Sack, MD, MPH1, Alexander Gusev, PhD1, Shilpa Grover, MD, MPH1
1Brigham and Women's Hospital, Boston, MA; 2Dana-Farber Cancer Institute, Boston, MA; 3Weil Cornell Medical College, New York, NY
Introduction: Immune-checkpoint inhibitors (ICIs) have improved survival and have become standard treatment for multiple cancer types. Immune-related adverse events (irAEs) including colitis can be severe and life-threatening. Genetic predisposition to irAEs and specifically colitis are poorly understood.
Methods: We included patients treated with ICIs across all cancer subtypes. irAEs were defined according to CTCAE v5.0. Patients with colitis were known to have biopsy-proven involvement. Data on use of biologics (vedolizumab or infliximab) for treatment of colitis were collected. We imputed common germline features from panel sequenced tumors. We investigated the influence of germline features on irAEs using multivariate and multistage survival analysis. We further analyzed the association between known polygenic risk scores (PRS) and the development of ICI colitis.
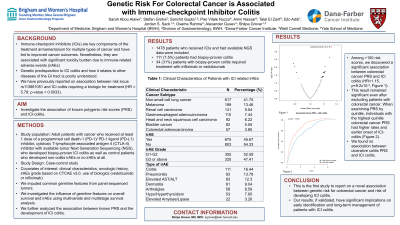
Results: 1478 patients who received ICIs were included. The most common cancer subtypes were non-small cell lung cancer (N=617, 41.7%), melanoma (N=199, 13.5%), and renal cell carcinoma (N=141, 9.5%). Of the 675 (45.7%) patients who developed any grade irAEs, 320 (47.4%) were ≥ grade 3. The most common irAEs were colitis (N=152, 22.5%), pneumonitis (N=93, 13.8%), and hepatitis (N=83, 12.3%). Of patients who developed ICI colitis, 99 (65.1%) were ≥ grade 3, and 34 (22.4%) required treatment with biologics. Among >100 risk scores, we discovered a very significant association between colorectal cancer PRS and ICI colitis (HR=1.15, p=9.2x10-4). This result remained significant even after excluding patients with colorectal cancer. When examining PRS by quintile, individuals with the highest quintile colorectal cancer PRS had higher rates and earlier onset of ICI-colitis (Figure). We found no association between ulcerative colitis PRS and ICI colitis.
Discussion: Our study is the first to report on a novel association between genetic risk for colorectal cancer and risk of developing ICI colitis. Our results, if validated, have significant implications on early identification and long-term management of patients with ICI colitis.

Disclosures:
Sarah Abou Alaiwi, MD1, Stefan Groha, PhD2, Sanchit Gupta, MD, MS1, Pier Vitale Nuzzo, MD, PhD3, Amin Nassar, MD1, Talal El Zarif, MD2, Elio Adib, MD2, Jordan Sack, MD, MPH1, Alexander Gusev, PhD1, Shilpa Grover, MD, MPH1. P1584 - Genetic Risk for Colorectal Cancer Is Associated With Earlier Onset and Higher Incidence of Immune Checkpoint Inhibitor Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brigham and Women's Hospital, Boston, MA; 2Dana-Farber Cancer Institute, Boston, MA; 3Weil Cornell Medical College, New York, NY
Introduction: Immune-checkpoint inhibitors (ICIs) have improved survival and have become standard treatment for multiple cancer types. Immune-related adverse events (irAEs) including colitis can be severe and life-threatening. Genetic predisposition to irAEs and specifically colitis are poorly understood.
Methods: We included patients treated with ICIs across all cancer subtypes. irAEs were defined according to CTCAE v5.0. Patients with colitis were known to have biopsy-proven involvement. Data on use of biologics (vedolizumab or infliximab) for treatment of colitis were collected. We imputed common germline features from panel sequenced tumors. We investigated the influence of germline features on irAEs using multivariate and multistage survival analysis. We further analyzed the association between known polygenic risk scores (PRS) and the development of ICI colitis.
Results: 1478 patients who received ICIs were included. The most common cancer subtypes were non-small cell lung cancer (N=617, 41.7%), melanoma (N=199, 13.5%), and renal cell carcinoma (N=141, 9.5%). Of the 675 (45.7%) patients who developed any grade irAEs, 320 (47.4%) were ≥ grade 3. The most common irAEs were colitis (N=152, 22.5%), pneumonitis (N=93, 13.8%), and hepatitis (N=83, 12.3%). Of patients who developed ICI colitis, 99 (65.1%) were ≥ grade 3, and 34 (22.4%) required treatment with biologics. Among >100 risk scores, we discovered a very significant association between colorectal cancer PRS and ICI colitis (HR=1.15, p=9.2x10-4). This result remained significant even after excluding patients with colorectal cancer. When examining PRS by quintile, individuals with the highest quintile colorectal cancer PRS had higher rates and earlier onset of ICI-colitis (Figure). We found no association between ulcerative colitis PRS and ICI colitis.
Discussion: Our study is the first to report on a novel association between genetic risk for colorectal cancer and risk of developing ICI colitis. Our results, if validated, have significant implications on early identification and long-term management of patients with ICI colitis.

Figure: Association between Colorectal Cancer Risk Polygenic Risk Score and ICI Colitis
Disclosures:
Sarah Abou Alaiwi indicated no relevant financial relationships.
Stefan Groha: GSK – Employee.
Sanchit Gupta: Bristol Myers Squibb – Consultant.
Pier Vitale Nuzzo indicated no relevant financial relationships.
Amin Nassar indicated no relevant financial relationships.
Talal El Zarif indicated no relevant financial relationships.
Elio Adib indicated no relevant financial relationships.
Jordan Sack indicated no relevant financial relationships.
Alexander Gusev indicated no relevant financial relationships.
Shilpa Grover indicated no relevant financial relationships.
Sarah Abou Alaiwi, MD1, Stefan Groha, PhD2, Sanchit Gupta, MD, MS1, Pier Vitale Nuzzo, MD, PhD3, Amin Nassar, MD1, Talal El Zarif, MD2, Elio Adib, MD2, Jordan Sack, MD, MPH1, Alexander Gusev, PhD1, Shilpa Grover, MD, MPH1. P1584 - Genetic Risk for Colorectal Cancer Is Associated With Earlier Onset and Higher Incidence of Immune Checkpoint Inhibitor Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
