Monday Poster Session
Category: Colon
P1587 - Diagnosis of Microscopic Colitis in Patients With Irritable Bowel Syndrome Subtype Diarrhea: A Case Control Propensity Matched Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Paul P. Hong, MD
Loyola University Medical Center
Chicago, IL
Presenting Author(s)
Ikponmwosa Enofe, MD, MPH1, Paul Hong, MD1, Michael Fayad, DO2, Ann O'neill, MD2, William Adams, PhD3, Xianzhong Ding, MD2, Ayokunle T.. Abegunde, MD2
1Loyola University Medical Center, Chicago, IL; 2Loyola University Medical Center, Maywood, IL; 3Loyola University, Chicago, IL
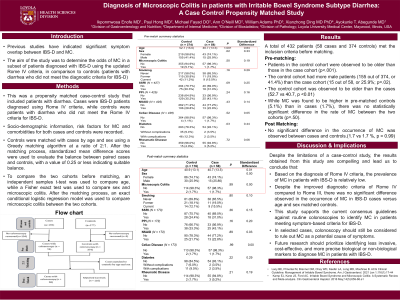
Introduction: Prior studies have suggested significant symptom overlap between IBS-D and MC. We aimed to determine the odds of MC in a subset of patients with a diagnosis of IBS-D using the updated Rome IV Criteria compared to controls (patients with diarrhea not meeting diagnostic criteria for IBS-D)
Methods: We conducted a propensity matched case-control study. Cases were IBS-D patients diagnosed by Rome IV criteria. Controls were patients with diarrhea that did not fulfill the Rome IV diagnostic criteria for IBS-D. We recorded information on patients’ socio-demographic, risk factors for MC and comorbidities for cases and controls. Only patients who had a colonoscopy were included in the analysis. Controls were matched with cases by age and sex using a Greedy 2:1 matching algorithm. An exact conditional logistic regression model was used to compare MC between the two cohorts.
Results: A pre-match total of 432 patients (cases n= 374, controls n =58) met inclusion criteria. Before matching (Tab 1), patients in the control cohort were older than patients in the case cohort (p < .001), and there were more male patients in the control cohort (n = 155/374 or 41.4%) than case cohort (n = 15/58 or 25.9%; p = .02). Despite higher occurrence of MC noted in pre-matched controls (5.1%) compared to cases (1.7%), there was no significant difference in the rate of MC between the two cohorts (p = .50). Following the matching algorithm (Fig2), the cases and controls were well balanced on age and sex (all standardized difference scores < 0.25) and there remained no difference in the rate of MC between the two cohorts (1.7 vs 1.7 %, p = .99)
Discussion: Prior studies using the Rome III criteria, showed no difference in occurrence of MC in IBS-D patients compared to age and sex matched controls. Although the Rome IV criteria was developed to address the shortcomings of Rome III, our study did not show a significant difference in the occurrence of MC in IBS-D cases compared to age and sex matched controls. Our results do not support the use of routine colonoscopy to evaluate for MC in IBS-D patients due to uncertain benefits and low prevalence of MC in IBS-D. However, in highly selected patients, colonoscopy should still be considered to rule out MC as a potential etiology for symptoms. Future research should focus on identifying less invasive, cost effective, and more precise biological or non-biological markers to diagnose MC in patients with IBS-D.
Disclosures:
Ikponmwosa Enofe, MD, MPH1, Paul Hong, MD1, Michael Fayad, DO2, Ann O'neill, MD2, William Adams, PhD3, Xianzhong Ding, MD2, Ayokunle T.. Abegunde, MD2. P1587 - Diagnosis of Microscopic Colitis in Patients With Irritable Bowel Syndrome Subtype Diarrhea: A Case Control Propensity Matched Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Loyola University Medical Center, Chicago, IL; 2Loyola University Medical Center, Maywood, IL; 3Loyola University, Chicago, IL
Introduction: Prior studies have suggested significant symptom overlap between IBS-D and MC. We aimed to determine the odds of MC in a subset of patients with a diagnosis of IBS-D using the updated Rome IV Criteria compared to controls (patients with diarrhea not meeting diagnostic criteria for IBS-D)
Methods: We conducted a propensity matched case-control study. Cases were IBS-D patients diagnosed by Rome IV criteria. Controls were patients with diarrhea that did not fulfill the Rome IV diagnostic criteria for IBS-D. We recorded information on patients’ socio-demographic, risk factors for MC and comorbidities for cases and controls. Only patients who had a colonoscopy were included in the analysis. Controls were matched with cases by age and sex using a Greedy 2:1 matching algorithm. An exact conditional logistic regression model was used to compare MC between the two cohorts.
Results: A pre-match total of 432 patients (cases n= 374, controls n =58) met inclusion criteria. Before matching (Tab 1), patients in the control cohort were older than patients in the case cohort (p < .001), and there were more male patients in the control cohort (n = 155/374 or 41.4%) than case cohort (n = 15/58 or 25.9%; p = .02). Despite higher occurrence of MC noted in pre-matched controls (5.1%) compared to cases (1.7%), there was no significant difference in the rate of MC between the two cohorts (p = .50). Following the matching algorithm (Fig2), the cases and controls were well balanced on age and sex (all standardized difference scores < 0.25) and there remained no difference in the rate of MC between the two cohorts (1.7 vs 1.7 %, p = .99)
Discussion: Prior studies using the Rome III criteria, showed no difference in occurrence of MC in IBS-D patients compared to age and sex matched controls. Although the Rome IV criteria was developed to address the shortcomings of Rome III, our study did not show a significant difference in the occurrence of MC in IBS-D cases compared to age and sex matched controls. Our results do not support the use of routine colonoscopy to evaluate for MC in IBS-D patients due to uncertain benefits and low prevalence of MC in IBS-D. However, in highly selected patients, colonoscopy should still be considered to rule out MC as a potential etiology for symptoms. Future research should focus on identifying less invasive, cost effective, and more precise biological or non-biological markers to diagnose MC in patients with IBS-D.
Disclosures:
Ikponmwosa Enofe indicated no relevant financial relationships.
Paul Hong indicated no relevant financial relationships.
Michael Fayad indicated no relevant financial relationships.
Ann O'neill indicated no relevant financial relationships.
William Adams indicated no relevant financial relationships.
Xianzhong Ding indicated no relevant financial relationships.
Ayokunle Abegunde indicated no relevant financial relationships.
Ikponmwosa Enofe, MD, MPH1, Paul Hong, MD1, Michael Fayad, DO2, Ann O'neill, MD2, William Adams, PhD3, Xianzhong Ding, MD2, Ayokunle T.. Abegunde, MD2. P1587 - Diagnosis of Microscopic Colitis in Patients With Irritable Bowel Syndrome Subtype Diarrhea: A Case Control Propensity Matched Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
