Monday Poster Session
Category: Colon
P1595 - A Comparative Analysis of Clostridium difficile Infection Outcomes in Hospitalizations With and Without Colorectal Cancer in the United States
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall

Fnu Vikash, MD
Albert Einstein College of Medicine, Jacobi Medical Center
Bronx, NY
Presenting Author(s)
Fnu Vikash, MD1, Sindhu Vikash, MD1, Vikash Kumar, MD2, Sobaan Taj, MD3, Chun-Wei Pan, MD4, Noor Syed, MD5, Rewanth Katamreddy, MD6, Sana Hussain, MD7, Dushyant Singh. Dahiya, MD8, Sunny Patel, MD9, Donald P.. Kotler, MD9
1Albert Einstein College of Medicine, Jacobi Medical Center, Bronx, NY; 2Brooklyn Hospital Center, Brooklyn, NY; 3Hackensack Meridian Jersey Shore University Medical Center, Neptune, NJ; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 5Santa Clara Valley Medical Center, San Jose, CA; 6Saint Michael’s Medical Center, Newark, NJ; 7Khyber Teaching Hospital, Peshawar, Northern Areas, Pakistan; 8University of Kansas School of Medicine, Kansas City, KS; 9Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY
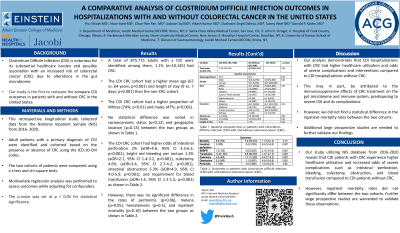
Introduction: Clostridium Difficile Infection (CDI) is notorious for its substantial healthcare burden and possible association with an increased risk of colorectal cancer (CRC) due to alterations in the gut microbiome. Our study aims to compare CDI outcomes in patients with and without CRC in the United States.
Methods: This retrospective longitudinal study collected data from the National Inpatient Sample (NIS) from 2016-2020. Adult patients with a primary diagnosis of CDI were identified and cohorted based on the presence or absence of CRC using the ICD-10-CM codes. The two cohorts of patients were compared using a t-test and chi-square tests. Multivariate regression analysis was performed to assess outcomes while adjusting for confounders. All p-values < 0.05 were statistically significant.
Results: A total of 875,775 adults with a CDI were identified; among them, 1.1% (n=10,145) had CRC. The CDI CRC cohort had a higher mean age (67 vs. 64 years; p=0.001) and length of stay (9 vs. 7 days; p=0.001) than the non-CRC cohort. The CDI CRC cohort had a higher proportion of Whites (74%; p=0.01) and males (47%; p=0.001). No statistical difference was noted in socioeconomic status (p=0.12) and geographic location (p=0.15) between the two groups (Table 1). The CDI CRC cohort had higher odds of intestinal perforation 2% (aOR=4.6, 95% CI 3.3-6.3, p=0.001), bright red bleeding per rectum 1.3% (aOR=2.1, 95% CI 1.4-3.2, p=0.001), colectomy 4.6% (aOR=3.4, 95% CI 2.7-4.2, p=0.001), intestinal obstruction 5.3% (aOR=4.9, 95% CI 4.0-5.9, p=0.001), and requirement for blood transfusion (aOR=1.4, 95% CI 1.2-1.5, p=0.001). However, there was no significant difference in the rates of peritonitis (p=0.06), melena (p=0.05), hematemesis (p=0.5), and inpatient mortality (p=0.10) between the two groups.
Discussion: Our analysis demonstrates that CDI hospitalizations with CRC had higher healthcare utilization and odds of severe complications and interventions compared to CDI hospitalizations without CRC. This may, in part, be attributed to the immunosuppressive effects of CRC treatment on the gut microbiome and immune system, predisposing to severe CDI and its complications. However, we did not find a statistical difference in the inpatient mortality rates between the two cohorts. Additional large prospective studies are needed to further validate our findings.
Disclosures:
Fnu Vikash, MD1, Sindhu Vikash, MD1, Vikash Kumar, MD2, Sobaan Taj, MD3, Chun-Wei Pan, MD4, Noor Syed, MD5, Rewanth Katamreddy, MD6, Sana Hussain, MD7, Dushyant Singh. Dahiya, MD8, Sunny Patel, MD9, Donald P.. Kotler, MD9. P1595 - A Comparative Analysis of Clostridium difficile Infection Outcomes in Hospitalizations With and Without Colorectal Cancer in the United States, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Albert Einstein College of Medicine, Jacobi Medical Center, Bronx, NY; 2Brooklyn Hospital Center, Brooklyn, NY; 3Hackensack Meridian Jersey Shore University Medical Center, Neptune, NJ; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 5Santa Clara Valley Medical Center, San Jose, CA; 6Saint Michael’s Medical Center, Newark, NJ; 7Khyber Teaching Hospital, Peshawar, Northern Areas, Pakistan; 8University of Kansas School of Medicine, Kansas City, KS; 9Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY
Introduction: Clostridium Difficile Infection (CDI) is notorious for its substantial healthcare burden and possible association with an increased risk of colorectal cancer (CRC) due to alterations in the gut microbiome. Our study aims to compare CDI outcomes in patients with and without CRC in the United States.
Methods: This retrospective longitudinal study collected data from the National Inpatient Sample (NIS) from 2016-2020. Adult patients with a primary diagnosis of CDI were identified and cohorted based on the presence or absence of CRC using the ICD-10-CM codes. The two cohorts of patients were compared using a t-test and chi-square tests. Multivariate regression analysis was performed to assess outcomes while adjusting for confounders. All p-values < 0.05 were statistically significant.
Results: A total of 875,775 adults with a CDI were identified; among them, 1.1% (n=10,145) had CRC. The CDI CRC cohort had a higher mean age (67 vs. 64 years; p=0.001) and length of stay (9 vs. 7 days; p=0.001) than the non-CRC cohort. The CDI CRC cohort had a higher proportion of Whites (74%; p=0.01) and males (47%; p=0.001). No statistical difference was noted in socioeconomic status (p=0.12) and geographic location (p=0.15) between the two groups (Table 1). The CDI CRC cohort had higher odds of intestinal perforation 2% (aOR=4.6, 95% CI 3.3-6.3, p=0.001), bright red bleeding per rectum 1.3% (aOR=2.1, 95% CI 1.4-3.2, p=0.001), colectomy 4.6% (aOR=3.4, 95% CI 2.7-4.2, p=0.001), intestinal obstruction 5.3% (aOR=4.9, 95% CI 4.0-5.9, p=0.001), and requirement for blood transfusion (aOR=1.4, 95% CI 1.2-1.5, p=0.001). However, there was no significant difference in the rates of peritonitis (p=0.06), melena (p=0.05), hematemesis (p=0.5), and inpatient mortality (p=0.10) between the two groups.
Discussion: Our analysis demonstrates that CDI hospitalizations with CRC had higher healthcare utilization and odds of severe complications and interventions compared to CDI hospitalizations without CRC. This may, in part, be attributed to the immunosuppressive effects of CRC treatment on the gut microbiome and immune system, predisposing to severe CDI and its complications. However, we did not find a statistical difference in the inpatient mortality rates between the two cohorts. Additional large prospective studies are needed to further validate our findings.
Disclosures:
Fnu Vikash indicated no relevant financial relationships.
Sindhu Vikash indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Sobaan Taj indicated no relevant financial relationships.
Chun-Wei Pan indicated no relevant financial relationships.
Noor Syed indicated no relevant financial relationships.
Rewanth Katamreddy indicated no relevant financial relationships.
Sana Hussain indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Sunny Patel indicated no relevant financial relationships.
Donald Kotler indicated no relevant financial relationships.
Fnu Vikash, MD1, Sindhu Vikash, MD1, Vikash Kumar, MD2, Sobaan Taj, MD3, Chun-Wei Pan, MD4, Noor Syed, MD5, Rewanth Katamreddy, MD6, Sana Hussain, MD7, Dushyant Singh. Dahiya, MD8, Sunny Patel, MD9, Donald P.. Kotler, MD9. P1595 - A Comparative Analysis of Clostridium difficile Infection Outcomes in Hospitalizations With and Without Colorectal Cancer in the United States, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
