Monday Poster Session
Category: Colon
P1604 - Practice Changes in Management of Gastrointestinal Immune-Related Adverse Events at a Tertiary Care Cancer Center
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
- MS
Malek Shatila, MD
University of Texas MD Anderson Cancer Center
Houston, Texas
Presenting Author(s)
Malek Shatila, MD1, Farzin Eshaghi, MD2, Austin Thomas, MD3, Andrew Kuang, MD2, Sidra Naz, MD, MPH1, Brandon Zhao, BSc4, Anusha Thomas, MD1, Hao Chi Zhang, MD1, Yinghong Wang, MD1
1University of Texas MD Anderson Cancer Center, Houston, TX; 2Baylor College of Medicine, Houston, TX; 3University of Texas Health Science Center at Houston, Houston, TX; 4Texas A&M, College Station, TX
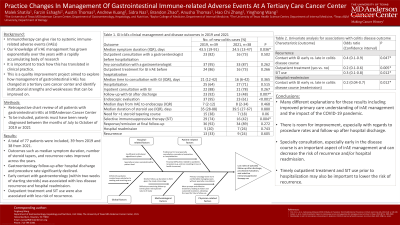
Introduction: Immunotherapy can give rise to systemic immune-related adverse events (irAEs) that are an obstacle to effective cancer treatment. Our understanding of this disease has evolved rapidly with extensive research over the years, and management guidelines are constantly updated. We aim to explore how management of gastrointestinal (GI) irAEs at a tertiary cancer care center has changed to identify areas for potential improvement.
Methods: This was a single-center, retrospective chart review of all patients with immune-mediated diarrhea and colitis (IMDC) from July to September of 2019 and 2021. The follow-up window was for up to a year after diagnosis. We collected data on patient demographics, clinical management, and disease course and outcomes.
Results: 77 patients were included in this study. We found worsening rates of GI specialty consultation (94.9% in 2019 vs. 86.8% in 2021), hospitalization (64.1% vs. 71.7%), follow-up after discharge (92.0% vs. 48.2%, p=0.007), endoscopic evaluation at baseline (94.8% vs. 60.5%, p< 0.001) and follow-up (38.9% vs. 27.2%), and selective immunosuppressive therapy (SIT) use (74.3% vs. 42.1%, p=0.004). Despite this, there was a marked improvement in outcomes including symptom duration (median 43.5 days in 2019 vs. 24.5 in 2021, p=0.036), need for >1 steroid tapering courses (38.5% vs. 18.5%, p=0.06), hospital readmission rates (53.1% vs. 33.3%), and colitis recurrence (36.1% vs. 28.0%) and remission rates (92.3% vs. 97.1%). This was true across different diarrhea and colitis CTCAE grades. The pooled data suggests that GI consultation prior to an event is significantly associated with lower readmission (p=0.000) and recurrence (p=0.001) rates, with earlier time to consultation also playing a role (p< 0.05). Finally, SIT use is also associated with less recurrence (OR: 0.3, p=0.012).
Discussion: This is one of the few qualitative studies exploring current practice in managing GI irAEs. Changes in practice between 2019 and 2021 likely reflect a variety of factors including an evolving knowledge of this disease as well as the impact of the COVID-19 pandemic. While overall disease outcomes are better in more recent years, there is room for improvement. Ensuring adequate and timely GI consultation and endoscopic evaluation rates, and more SIT use could help reduce hospital readmission and disease recurrence. Together, these findings can help improve the quality of GI irAE management algorithms at our institution.
Disclosures:
Malek Shatila, MD1, Farzin Eshaghi, MD2, Austin Thomas, MD3, Andrew Kuang, MD2, Sidra Naz, MD, MPH1, Brandon Zhao, BSc4, Anusha Thomas, MD1, Hao Chi Zhang, MD1, Yinghong Wang, MD1. P1604 - Practice Changes in Management of Gastrointestinal Immune-Related Adverse Events at a Tertiary Care Cancer Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas MD Anderson Cancer Center, Houston, TX; 2Baylor College of Medicine, Houston, TX; 3University of Texas Health Science Center at Houston, Houston, TX; 4Texas A&M, College Station, TX
Introduction: Immunotherapy can give rise to systemic immune-related adverse events (irAEs) that are an obstacle to effective cancer treatment. Our understanding of this disease has evolved rapidly with extensive research over the years, and management guidelines are constantly updated. We aim to explore how management of gastrointestinal (GI) irAEs at a tertiary cancer care center has changed to identify areas for potential improvement.
Methods: This was a single-center, retrospective chart review of all patients with immune-mediated diarrhea and colitis (IMDC) from July to September of 2019 and 2021. The follow-up window was for up to a year after diagnosis. We collected data on patient demographics, clinical management, and disease course and outcomes.
Results: 77 patients were included in this study. We found worsening rates of GI specialty consultation (94.9% in 2019 vs. 86.8% in 2021), hospitalization (64.1% vs. 71.7%), follow-up after discharge (92.0% vs. 48.2%, p=0.007), endoscopic evaluation at baseline (94.8% vs. 60.5%, p< 0.001) and follow-up (38.9% vs. 27.2%), and selective immunosuppressive therapy (SIT) use (74.3% vs. 42.1%, p=0.004). Despite this, there was a marked improvement in outcomes including symptom duration (median 43.5 days in 2019 vs. 24.5 in 2021, p=0.036), need for >1 steroid tapering courses (38.5% vs. 18.5%, p=0.06), hospital readmission rates (53.1% vs. 33.3%), and colitis recurrence (36.1% vs. 28.0%) and remission rates (92.3% vs. 97.1%). This was true across different diarrhea and colitis CTCAE grades. The pooled data suggests that GI consultation prior to an event is significantly associated with lower readmission (p=0.000) and recurrence (p=0.001) rates, with earlier time to consultation also playing a role (p< 0.05). Finally, SIT use is also associated with less recurrence (OR: 0.3, p=0.012).
Discussion: This is one of the few qualitative studies exploring current practice in managing GI irAEs. Changes in practice between 2019 and 2021 likely reflect a variety of factors including an evolving knowledge of this disease as well as the impact of the COVID-19 pandemic. While overall disease outcomes are better in more recent years, there is room for improvement. Ensuring adequate and timely GI consultation and endoscopic evaluation rates, and more SIT use could help reduce hospital readmission and disease recurrence. Together, these findings can help improve the quality of GI irAE management algorithms at our institution.
Disclosures:
Malek Shatila indicated no relevant financial relationships.
Farzin Eshaghi indicated no relevant financial relationships.
Austin Thomas indicated no relevant financial relationships.
Andrew Kuang indicated no relevant financial relationships.
Sidra Naz indicated no relevant financial relationships.
Brandon Zhao indicated no relevant financial relationships.
Anusha Thomas indicated no relevant financial relationships.
Hao Chi Zhang indicated no relevant financial relationships.
Yinghong Wang: ilyapharma – Consultant. IOTA – Consultant. Janssen – Consultant. MabQuest – Advisory Committee/Board Member. Sorriso – Consultant. Tillotts – Consultant.
Malek Shatila, MD1, Farzin Eshaghi, MD2, Austin Thomas, MD3, Andrew Kuang, MD2, Sidra Naz, MD, MPH1, Brandon Zhao, BSc4, Anusha Thomas, MD1, Hao Chi Zhang, MD1, Yinghong Wang, MD1. P1604 - Practice Changes in Management of Gastrointestinal Immune-Related Adverse Events at a Tertiary Care Cancer Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
