Monday Poster Session
Category: Colon
P1617 - The Incidence and Severity of Inpatient Hospital Admissions for Concomitant COVID-19 and Clostridioides difficile Infection
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Megan B. Ghai, MD, MPH, MA
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Megan B. Ghai, MD, MPH, MA1, Pooja Rangan, MBBS, MPH1, Wahid Wassef, MD, MPH, FACG2
1University of Arizona College of Medicine, Phoenix, AZ; 2Banner University Medical Center, Phoenix, AZ
Introduction: More than 10% of those with COVID-19 experienced diarrhea. While it is hypothesized that COVID-19 causes cell-mediated changes in the intestine leading to diarrhea, co-infections with Clostridioides difficile have also been reported. Here we compare the incidence and severity of hospitalizations for Clostridioides difficile infection (CDI) in those with and without a concomitant diagnosis of COVID-19.
Methods: A retrospective analysis of U.S. inpatient discharges from 2020 using the Healthcare Cost and Utilization Project National Inpatient Sample was performed. Included were adult CDI discharges, as defined by ICD-10-CM codes. Weights were used to generate nationally representative estimates. Descriptive statistics were produced using Pearson’s chi-squared tests. Severity was evaluated, as defined by mean length of stay (LOS), mortality, and complication rates. Multivariate logistic regression was used to evaluate the independent association of COVID-19 and death within the CDI population.
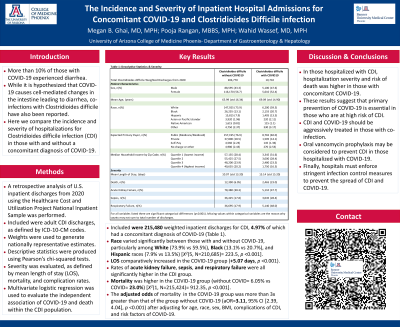
Results: Included were 215,480 weighted inpatient discharges for CDI, 4.97% of which had a concomitant diagnosis of COVID-19 (Table 1). Race varied significantly between those with and without COVID-19, particularly among White (73.9% vs 59.5%), Black (13.1% vs 20.7%), and Hispanic races (7.9% vs 13.5%) [X2(5, N=210,685)= 223.5, p < 0.001]. LOS comparatively increased in the COVID-19 group (+5.07 days, p < 0.001). Rates of acute kidney failure, sepsis, and respiratory failure were all significantly higher in the CDI group. Death rate was higher in the COVID-19 group (without COVID= 6.05% vs COVID= 23.0%) [X2(1, N=215,424)= 912.35, p < 0.001]. The adjusted odds of death in the COVID-19 group was more than three times greater than that of the group without COVID-19 (OR=3.11, 95% CI [2.39, 4.04], p < 0.001) after adjusting for age, race, sex, BMI, complications of CDI, and risk factors for developing worsening COVID-19.
Discussion: In those hospitalized with CDI, hospitalization severity and risk of death was higher in those with concomitant COVID-19. These results suggest that primary prevention of COVID-19 is essential in those who are at high risk of CDI. CDI and COVID-19 should be aggressively treated in those with co-infection. Oral vancomycin prophylaxis may be considered to prevent CDI in those hospitalized with COVID-19. Finally, hospitals must enforce stringent infection control measures to prevent the spread of CDI and COVID-19.
Disclosures:
Megan B. Ghai, MD, MPH, MA1, Pooja Rangan, MBBS, MPH1, Wahid Wassef, MD, MPH, FACG2. P1617 - The Incidence and Severity of Inpatient Hospital Admissions for Concomitant COVID-19 and Clostridioides difficile Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, AZ; 2Banner University Medical Center, Phoenix, AZ
Introduction: More than 10% of those with COVID-19 experienced diarrhea. While it is hypothesized that COVID-19 causes cell-mediated changes in the intestine leading to diarrhea, co-infections with Clostridioides difficile have also been reported. Here we compare the incidence and severity of hospitalizations for Clostridioides difficile infection (CDI) in those with and without a concomitant diagnosis of COVID-19.
Methods: A retrospective analysis of U.S. inpatient discharges from 2020 using the Healthcare Cost and Utilization Project National Inpatient Sample was performed. Included were adult CDI discharges, as defined by ICD-10-CM codes. Weights were used to generate nationally representative estimates. Descriptive statistics were produced using Pearson’s chi-squared tests. Severity was evaluated, as defined by mean length of stay (LOS), mortality, and complication rates. Multivariate logistic regression was used to evaluate the independent association of COVID-19 and death within the CDI population.
Results: Included were 215,480 weighted inpatient discharges for CDI, 4.97% of which had a concomitant diagnosis of COVID-19 (Table 1). Race varied significantly between those with and without COVID-19, particularly among White (73.9% vs 59.5%), Black (13.1% vs 20.7%), and Hispanic races (7.9% vs 13.5%) [X2(5, N=210,685)= 223.5, p < 0.001]. LOS comparatively increased in the COVID-19 group (+5.07 days, p < 0.001). Rates of acute kidney failure, sepsis, and respiratory failure were all significantly higher in the CDI group. Death rate was higher in the COVID-19 group (without COVID= 6.05% vs COVID= 23.0%) [X2(1, N=215,424)= 912.35, p < 0.001]. The adjusted odds of death in the COVID-19 group was more than three times greater than that of the group without COVID-19 (OR=3.11, 95% CI [2.39, 4.04], p < 0.001) after adjusting for age, race, sex, BMI, complications of CDI, and risk factors for developing worsening COVID-19.
Discussion: In those hospitalized with CDI, hospitalization severity and risk of death was higher in those with concomitant COVID-19. These results suggest that primary prevention of COVID-19 is essential in those who are at high risk of CDI. CDI and COVID-19 should be aggressively treated in those with co-infection. Oral vancomycin prophylaxis may be considered to prevent CDI in those hospitalized with COVID-19. Finally, hospitals must enforce stringent infection control measures to prevent the spread of CDI and COVID-19.
Disclosures:
Megan Ghai indicated no relevant financial relationships.
Pooja Rangan indicated no relevant financial relationships.
Wahid Wassef indicated no relevant financial relationships.
Megan B. Ghai, MD, MPH, MA1, Pooja Rangan, MBBS, MPH1, Wahid Wassef, MD, MPH, FACG2. P1617 - The Incidence and Severity of Inpatient Hospital Admissions for Concomitant COVID-19 and Clostridioides difficile Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
