Monday Poster Session
Category: Colon
P1639 - An Unusual Presentation of Ischemic Colitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Rafaela Izurieta, MD
Brooke Army Medical Center
San Antonio, TX
Presenting Author(s)
Rafaela Izurieta, MD, Cassandra Craig, MD, Douglas Walton, MD
Brooke Army Medical Center, San Antonio, TX
Introduction: Ischemic Colitis (IC) is the most common type of gastrointestinal vascular disease, occurring in 15.6-17.7 cases per 100,000 persons per year. Many etiologies of IC exist, but in all cases, there is an element of local hypoperfusion leading to hypoxia. IC occurs most often in the watershed areas, so-called because of the lack of collateral vascularity in these zones. The most common demographic of patients afflicted are females over the age of 60. Common presenting symptoms are abdominal pain and lower gastrointestinal bleeding. We present a case of IC in a young man with discordant imaging and colonoscopy findings.
Case Description/Methods: A 38-year-old man with history of type 1 diabetes (DM1) and obesity presented to the ER for abdominal pain and hematochezia. He had recently completed a 7-day course of antibiotics and ibuprofen 600mg every 6 hours after a periodontal procedure. Physical exam demonstrated mild tachycardia and minor diffuse abdominal tenderness without distension. Labs were notable for WBC 11k, CRP 1.4 mg/dl, normal electrolytes/Hgb/fecal calprotectin, and negative infectious stool studies. Abdominal CT scan showed diffuse mural thickening of the entire colon with mild associated mesenteric fat stranding. Colonoscopy revealed erythema and superficial ulcerations in the transverse/descending colon and rectum, with sparing of the sigmoid colon. A classic stripe sign was visualized in the rectum. Targeted biopsies demonstrated an ischemic pattern, with pathology comment that this was likely true IC versus drug effect.
Discussion: IC should not only be considered in the older female population with vascular disease and a period of local hypoperfusion, but also in cases like this. Poorly controlled DM1, as in patient’s case, predisposes to vascular disease and may be exquisitely sensitive to tissue ischemia driven by even short courses of NSAID use. CT scans can often mislead the unsuspecting eye into an alternative diagnosis; however, our colonoscopy confirmed a watershed distribution and ischemic changes on tissue biopsy.
We highlight this case because of an unusual presentation of a relatively common gastroenterology diagnosis. We suspect there was a two-hit phenomenon with NSAID-induced ischemia driving true ischemia in a young poorly controlled diabetic with underlying vascular disease. With the obesity epidemic on the rise and ubiquitous NSAID use, this type of presentation will likely become more common and thus important for gastroenterologists to recognize.

Disclosures:
Rafaela Izurieta, MD, Cassandra Craig, MD, Douglas Walton, MD. P1639 - An Unusual Presentation of Ischemic Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Brooke Army Medical Center, San Antonio, TX
Introduction: Ischemic Colitis (IC) is the most common type of gastrointestinal vascular disease, occurring in 15.6-17.7 cases per 100,000 persons per year. Many etiologies of IC exist, but in all cases, there is an element of local hypoperfusion leading to hypoxia. IC occurs most often in the watershed areas, so-called because of the lack of collateral vascularity in these zones. The most common demographic of patients afflicted are females over the age of 60. Common presenting symptoms are abdominal pain and lower gastrointestinal bleeding. We present a case of IC in a young man with discordant imaging and colonoscopy findings.
Case Description/Methods: A 38-year-old man with history of type 1 diabetes (DM1) and obesity presented to the ER for abdominal pain and hematochezia. He had recently completed a 7-day course of antibiotics and ibuprofen 600mg every 6 hours after a periodontal procedure. Physical exam demonstrated mild tachycardia and minor diffuse abdominal tenderness without distension. Labs were notable for WBC 11k, CRP 1.4 mg/dl, normal electrolytes/Hgb/fecal calprotectin, and negative infectious stool studies. Abdominal CT scan showed diffuse mural thickening of the entire colon with mild associated mesenteric fat stranding. Colonoscopy revealed erythema and superficial ulcerations in the transverse/descending colon and rectum, with sparing of the sigmoid colon. A classic stripe sign was visualized in the rectum. Targeted biopsies demonstrated an ischemic pattern, with pathology comment that this was likely true IC versus drug effect.
Discussion: IC should not only be considered in the older female population with vascular disease and a period of local hypoperfusion, but also in cases like this. Poorly controlled DM1, as in patient’s case, predisposes to vascular disease and may be exquisitely sensitive to tissue ischemia driven by even short courses of NSAID use. CT scans can often mislead the unsuspecting eye into an alternative diagnosis; however, our colonoscopy confirmed a watershed distribution and ischemic changes on tissue biopsy.
We highlight this case because of an unusual presentation of a relatively common gastroenterology diagnosis. We suspect there was a two-hit phenomenon with NSAID-induced ischemia driving true ischemia in a young poorly controlled diabetic with underlying vascular disease. With the obesity epidemic on the rise and ubiquitous NSAID use, this type of presentation will likely become more common and thus important for gastroenterologists to recognize.

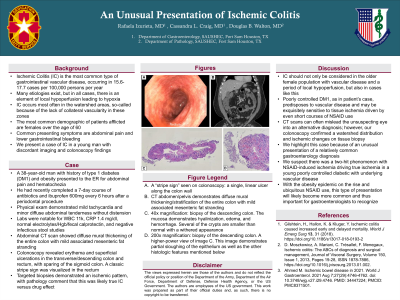
Figure: A. CT abdomen/pelvis demonstrates diffuse mural thickening/stratification of the entire colon with mild associated mesenteric fat stranding.
B. A “stripe sign” seen on colonoscopy: a single, linear ulcer along the colon wall.
C. 200x magnification: biopsy of the descending colon. A higher-power view of image D. This image demonstrates partial sloughing of the epithelium as well as the other histologic features mentioned below.
D. 40x magnification: biopsy of the descending colon. The mucosa demonstrates hyalinization, edema, and hemorrhage. Several of the crypts are smaller than normal with a withered appearance.
B. A “stripe sign” seen on colonoscopy: a single, linear ulcer along the colon wall.
C. 200x magnification: biopsy of the descending colon. A higher-power view of image D. This image demonstrates partial sloughing of the epithelium as well as the other histologic features mentioned below.
D. 40x magnification: biopsy of the descending colon. The mucosa demonstrates hyalinization, edema, and hemorrhage. Several of the crypts are smaller than normal with a withered appearance.
Disclosures:
Rafaela Izurieta indicated no relevant financial relationships.
Cassandra Craig indicated no relevant financial relationships.
Douglas Walton indicated no relevant financial relationships.
Rafaela Izurieta, MD, Cassandra Craig, MD, Douglas Walton, MD. P1639 - An Unusual Presentation of Ischemic Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
