Monday Poster Session
Category: Colon
P1643 - Secondary Extramedullary Plasmacytoma - A Rare Entity Affecting Appendix, Colon, and Pancreas: A Report of Two Cases
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall

Sharifeh Almasaid, MD
SUNY Upstate University Hospital
Syracuse, NY
Presenting Author(s)
Sharifeh Almasaid, MD1, Gayatri Pemmasani, MBBS2, Pujitha kudaravalli, MBBS3, Hatem al Kashroom, MBBS1, Ganesh Aswath, MD2
1SUNY Upstate University Hospital, Syracuse, NY; 2Upstate University Hospital, Syracuse, NY; 3SUNY Upstate Medical University, Syracuse, NY
Introduction: Plasma cell neoplasms can proliferate outside the bone marrow and develop into soft tissue plasmacytomas, which are more aggressive and have worse prognosis compared to multiple myeloma (MM). These can lose contact with the bone and spread hematogenously as extramedullary plasmacytomas (EMP), which are commonly observed in the head and neck. In this discussion, we focus on two rare cases of EMP involving the gastrointestinal (GI) tract.
Case Description/Methods: Case 1: An 80-year-old male with a history of solitary aggressive plasmacytoma developed acute-on-chronic anemia. EGD revealed a large malignant-looking duodenal ulcer and two small masses on the duodenal wall. Colonoscopy showed a malignant tumor adjacent to the appendiceal orifice, a submucosal ulcerated nodule with malignant features in the ascending colon, and a cecal polyp. Histological examination of these lesions confirmed plasma cell myeloma with a plasmablastic morphology. The patient was later admitted for small bowel obstruction and underwent exploratory laparotomy with bowel resection. Histology of the excised intestine revealed a plasma cell neoplasm with a plasmablastic morphology.
Case 2: A 75-year-old female with a history of metastatic MM presented with abdominal pain. Abdominopelvic CT imaging showed fullness of the pancreatic head without a definite mass. MRI of the abdomen identified a 3.5 cm mass. Endoscopic ultrasound guided tissue biopsy demonstrated a plasma cell dyscrasia consistent with metastatic MM. A week later, she experienced worsening abdominal pain. Repeat imaging showed increase in the pancreatic mass and new focal wall thickening in the ascending colon near the cecum. Chemotherapy was initiated, however, the patient deteriorated and died.
Discussion: EMP occurrence in the GI tract is relatively rare with 4-5% of all cases. The small intestine is the most common affected site, while colon and pancreas involvement are rare. EMP could be suspected on imaging studies, but a definite tissue biopsy is needed to establish the diagnosis. Appendix involvement by EMP was first reported in 2020, and here, we present the second case to best of our knowledge. Pancreatic involvement was reported in nearly 25 cases, and the head is the most affected.
EMP involvement in the GI tract is rare and the clinical course is unknown. Guidelines for its diagnosis and management have not yet been established. However, early detection and a multidisciplinary approach to management are vital for improving prognosis.

Disclosures:
Sharifeh Almasaid, MD1, Gayatri Pemmasani, MBBS2, Pujitha kudaravalli, MBBS3, Hatem al Kashroom, MBBS1, Ganesh Aswath, MD2. P1643 - Secondary Extramedullary Plasmacytoma - A Rare Entity Affecting Appendix, Colon, and Pancreas: A Report of Two Cases, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1SUNY Upstate University Hospital, Syracuse, NY; 2Upstate University Hospital, Syracuse, NY; 3SUNY Upstate Medical University, Syracuse, NY
Introduction: Plasma cell neoplasms can proliferate outside the bone marrow and develop into soft tissue plasmacytomas, which are more aggressive and have worse prognosis compared to multiple myeloma (MM). These can lose contact with the bone and spread hematogenously as extramedullary plasmacytomas (EMP), which are commonly observed in the head and neck. In this discussion, we focus on two rare cases of EMP involving the gastrointestinal (GI) tract.
Case Description/Methods: Case 1: An 80-year-old male with a history of solitary aggressive plasmacytoma developed acute-on-chronic anemia. EGD revealed a large malignant-looking duodenal ulcer and two small masses on the duodenal wall. Colonoscopy showed a malignant tumor adjacent to the appendiceal orifice, a submucosal ulcerated nodule with malignant features in the ascending colon, and a cecal polyp. Histological examination of these lesions confirmed plasma cell myeloma with a plasmablastic morphology. The patient was later admitted for small bowel obstruction and underwent exploratory laparotomy with bowel resection. Histology of the excised intestine revealed a plasma cell neoplasm with a plasmablastic morphology.
Case 2: A 75-year-old female with a history of metastatic MM presented with abdominal pain. Abdominopelvic CT imaging showed fullness of the pancreatic head without a definite mass. MRI of the abdomen identified a 3.5 cm mass. Endoscopic ultrasound guided tissue biopsy demonstrated a plasma cell dyscrasia consistent with metastatic MM. A week later, she experienced worsening abdominal pain. Repeat imaging showed increase in the pancreatic mass and new focal wall thickening in the ascending colon near the cecum. Chemotherapy was initiated, however, the patient deteriorated and died.
Discussion: EMP occurrence in the GI tract is relatively rare with 4-5% of all cases. The small intestine is the most common affected site, while colon and pancreas involvement are rare. EMP could be suspected on imaging studies, but a definite tissue biopsy is needed to establish the diagnosis. Appendix involvement by EMP was first reported in 2020, and here, we present the second case to best of our knowledge. Pancreatic involvement was reported in nearly 25 cases, and the head is the most affected.
EMP involvement in the GI tract is rare and the clinical course is unknown. Guidelines for its diagnosis and management have not yet been established. However, early detection and a multidisciplinary approach to management are vital for improving prognosis.

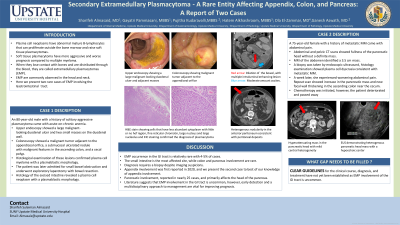
Figure: Figure [1] – Case 1
Image (A): Non-obstructing non-bleeding cratered duodenal ulcer found in the third portion of the duodenum. There is no evidence of perforation. Likely etiology is malignant in nature.
Image (B): 5 mm polyp in the cecum
Figure [2] – Case 1
Image (A): Axial image of CT A/P with IV contrast at the level of the cecum. The blue arrow shows a dilated small bowel loop with surrounding free fluid. Red arrow shows dilated appendiceal wall with surrounding fluid.
Image (B): Coronal image of CT A/P with IV and oral contrast. The red arrow shows thickening and mass of the distal small bowel with moderate amount of free fluid. Blue arrows show prominent small bowel loops secondary to the small bowel obstruction.
Figure [3] (A, B, C, D, E, F)
Histopathology slides for case 1 consistent with plasma cell neoplasm
Figure [4] – Case 2
Image (A): axial image of CT A/P with IV contrast. The red arrow shows a mass in the pancreatic head without definite borders.
Image (B): axial MRI subtraction image in the arterial phase. Red arrows show pancreatic head mass shows heterogenous enhancement
Figure [5] – Case 2
EUS image showing pancreatic head mass
Figure [6] (A, B, C, D)
Histopathology slides for case 2 consistent with plasma cell dyscrasia
Image (A): Non-obstructing non-bleeding cratered duodenal ulcer found in the third portion of the duodenum. There is no evidence of perforation. Likely etiology is malignant in nature.
Image (B): 5 mm polyp in the cecum
Figure [2] – Case 1
Image (A): Axial image of CT A/P with IV contrast at the level of the cecum. The blue arrow shows a dilated small bowel loop with surrounding free fluid. Red arrow shows dilated appendiceal wall with surrounding fluid.
Image (B): Coronal image of CT A/P with IV and oral contrast. The red arrow shows thickening and mass of the distal small bowel with moderate amount of free fluid. Blue arrows show prominent small bowel loops secondary to the small bowel obstruction.
Figure [3] (A, B, C, D, E, F)
Histopathology slides for case 1 consistent with plasma cell neoplasm
Figure [4] – Case 2
Image (A): axial image of CT A/P with IV contrast. The red arrow shows a mass in the pancreatic head without definite borders.
Image (B): axial MRI subtraction image in the arterial phase. Red arrows show pancreatic head mass shows heterogenous enhancement
Figure [5] – Case 2
EUS image showing pancreatic head mass
Figure [6] (A, B, C, D)
Histopathology slides for case 2 consistent with plasma cell dyscrasia
Disclosures:
Sharifeh Almasaid indicated no relevant financial relationships.
Gayatri Pemmasani indicated no relevant financial relationships.
Pujitha kudaravalli indicated no relevant financial relationships.
Hatem al Kashroom indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Sharifeh Almasaid, MD1, Gayatri Pemmasani, MBBS2, Pujitha kudaravalli, MBBS3, Hatem al Kashroom, MBBS1, Ganesh Aswath, MD2. P1643 - Secondary Extramedullary Plasmacytoma - A Rare Entity Affecting Appendix, Colon, and Pancreas: A Report of Two Cases, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
