Monday Poster Session
Category: Colon
P1648 - Lyme Disease Manifesting as Inflammatory Bowel Disease
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Makynzee B. Cantrell, BS
Lincoln Memorial University - DeBusk College of Osteopathic Medicine
Cumberland Gap, TN
Presenting Author(s)
Award: Presidential Poster Award
Makynzee B. Cantrell, BS1, Arundeep Kahlon, MBBS, MD2, Madalyn Thompson, BS3
1Lincoln Memorial University - DeBusk College of Osteopathic Medicine, Jewell Ridge, VA; 2Clinch Valley Medical Center, Richlands, VA; 3Lincoln Memorial University - DeBusk College of Osteopathic Medicine, Knoxville, TN
Introduction: Lyme disease is the most common tick-borne illness in the United States. It can involve multiple organ systems and produce a wide range of symptoms. Here we present a unique case of Lyme disease involving the GI system, where the patient presented with signs and symptoms of inflammatory bowel disease.
Case Description/Methods: A 39-year-old Caucasian male presented to the hospital with symptoms of generalized abdominal pain and bloody diarrhea, which started approximately one week prior. The patient denied any travel history or sick contacts. Physical exam revealed a fever of 101°F. The patient had mild, generalized abdominal tenderness without any peritoneal signs. Labs revealed WBCs to be within normal range, borderline anemia with hemoglobin 13 g/dl, and elevated CRP at 13.7 mg/L. Stool studies were negative for infection. A CT scan of the abdomen and pelvis with contrast showed findings suggestive of left-sided colitis.
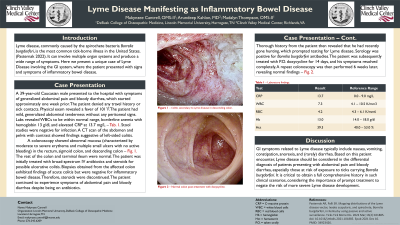
Subsequently, a colonoscopy showed abnormal mucosa (characterized by moderate to severe erythema and multiple small ulcers with no active bleeding) in the rectum, sigmoid colon, and descending colon; the rest of the colon and terminal ileum were normal. The patient was initially treated with broad-spectrum IV antibiotics and steroids for possible ulcerative colitis. Biopsies obtained from the affected colon exhibited findings of acute colitis but were negative for inflammatory bowel disease. Therefore, steroids were discontinued. The patient continued to experience symptoms of abdominal pain and bloody diarrhea despite being on antibiotics.
Thorough history from the patient then revealed that he had recently gone hunting, which triggered testing for Lyme Disease. Serology came back positive for Lyme antibodies. The patient was subsequently treated with P.O. doxycycline for 14 days, and his symptoms resolved completely. A repeat colonoscopy was then performed 6 weeks later which revealed normal findings.
Discussion: GI symptoms related to Lyme disease typically include nausea, vomiting, constipation, anorexia, and (rarely) diarrhea. Based on this patient encounter, Lyme disease should be considered in the differential diagnosis of patients presenting with abdominal pain and bloody diarrhea, especially those at risk of exposure to ticks carrying Lyme disease. It is critical to obtain a full comprehensive history in such clinical scenarios, considering the importance of prompt treatment to negate the risk of more severe Lyme disease development.

Disclosures:
Makynzee B. Cantrell, BS1, Arundeep Kahlon, MBBS, MD2, Madalyn Thompson, BS3. P1648 - Lyme Disease Manifesting as Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Makynzee B. Cantrell, BS1, Arundeep Kahlon, MBBS, MD2, Madalyn Thompson, BS3
1Lincoln Memorial University - DeBusk College of Osteopathic Medicine, Jewell Ridge, VA; 2Clinch Valley Medical Center, Richlands, VA; 3Lincoln Memorial University - DeBusk College of Osteopathic Medicine, Knoxville, TN
Introduction: Lyme disease is the most common tick-borne illness in the United States. It can involve multiple organ systems and produce a wide range of symptoms. Here we present a unique case of Lyme disease involving the GI system, where the patient presented with signs and symptoms of inflammatory bowel disease.
Case Description/Methods: A 39-year-old Caucasian male presented to the hospital with symptoms of generalized abdominal pain and bloody diarrhea, which started approximately one week prior. The patient denied any travel history or sick contacts. Physical exam revealed a fever of 101°F. The patient had mild, generalized abdominal tenderness without any peritoneal signs. Labs revealed WBCs to be within normal range, borderline anemia with hemoglobin 13 g/dl, and elevated CRP at 13.7 mg/L. Stool studies were negative for infection. A CT scan of the abdomen and pelvis with contrast showed findings suggestive of left-sided colitis.
Subsequently, a colonoscopy showed abnormal mucosa (characterized by moderate to severe erythema and multiple small ulcers with no active bleeding) in the rectum, sigmoid colon, and descending colon; the rest of the colon and terminal ileum were normal. The patient was initially treated with broad-spectrum IV antibiotics and steroids for possible ulcerative colitis. Biopsies obtained from the affected colon exhibited findings of acute colitis but were negative for inflammatory bowel disease. Therefore, steroids were discontinued. The patient continued to experience symptoms of abdominal pain and bloody diarrhea despite being on antibiotics.
Thorough history from the patient then revealed that he had recently gone hunting, which triggered testing for Lyme Disease. Serology came back positive for Lyme antibodies. The patient was subsequently treated with P.O. doxycycline for 14 days, and his symptoms resolved completely. A repeat colonoscopy was then performed 6 weeks later which revealed normal findings.
Discussion: GI symptoms related to Lyme disease typically include nausea, vomiting, constipation, anorexia, and (rarely) diarrhea. Based on this patient encounter, Lyme disease should be considered in the differential diagnosis of patients presenting with abdominal pain and bloody diarrhea, especially those at risk of exposure to ticks carrying Lyme disease. It is critical to obtain a full comprehensive history in such clinical scenarios, considering the importance of prompt treatment to negate the risk of more severe Lyme disease development.

Figure: A) Colitis secondary to Lyme disease in descending colon.
B) Normal colon post-treatment with doxycycline.
B) Normal colon post-treatment with doxycycline.
Disclosures:
Makynzee Cantrell indicated no relevant financial relationships.
Arundeep Kahlon indicated no relevant financial relationships.
Madalyn Thompson indicated no relevant financial relationships.
Makynzee B. Cantrell, BS1, Arundeep Kahlon, MBBS, MD2, Madalyn Thompson, BS3. P1648 - Lyme Disease Manifesting as Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

