Monday Poster Session
Category: Colon
P1650 - A Fatal Case of Cryoglobulinemic Vasculitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Jennifer Claytor, MD
Mount Sinai Hospital
New York, NY
Presenting Author(s)
Jennifer Claytor, MD1, David Greenwald, MD2
1Mount Sinai Hospital, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Cryoglobulinemic Vasculitis (CV) is rare; prior to effective antivirals, 90% of cases co-occurred with Hepatitis C. In patients with Sjogren’s Syndrome (SS), lymphoma, or other rheumatologic disorders, CV can be an unusual cause of catastrophic gastrointestinal (GI) hemorrhage and ischemia.
Case Description/Methods: A 74-year-old woman with SS on steroids and chronic kidney disease (CKD) IV due to cryoglobulinemic glomerulonephritis (GN) presented with melena and abdominal distension. She had mild renal and hepatic injury; negative Hepatitis B and C studies; and no further melena in the hospital. CT showed a single loop of thickened small bowel, 2 hepatic masses, and a pericardial effusion, “highly concerning for lymphoma or other malignancy”. She was transferred for possible balloon enteroscopy.
Push enteroscopy showed a violaceous, necrotic, obstructing mass and severe duodenitis in D3-4, favoring GI lymphoma over atypical infection and ischemia. Pathology showed acute on chronic duodenitis with sloughed epithelium. Flow cytometry was mostly acellular, with no clear evidence of lymphoma. Not having started outpatient rituximab and now acutely ill, she had anuric renal failure. ANA was strongly positive; RF, elevated, and C4, undetectable. Serum cryoglobulins were negative. She developed acute hematochezia.
EGD and colonoscopy were performed. The violaceous duodenal mass had disappeared, although granularity and erythema persisted. There were large ulcers in the rectum; a long, linear ulceration in the descending colon; and a purulent, ulcer bed >4cm in diameter obscuring the cecum. Pathology showed severely active nonspecific colitis, multifocal crypt injury, and neovascularization. Pulse steroids were started for presumed GI CV. On day 4, she developed with dual-pressor shock and had bacteremia, precluding plasmapheresis. Repeat CT showed infarctions of the spleen, kidneys, and liver. With worsening septic shock, she experienced PEA arrest and died.
Discussion: GI CV is rare and potentially fatal. Serum cryoglobulin testing is unreliable, with many false negatives due to incubation and collection error; low C4 and high RF are more typical. Older age, pulmonary or GI involvement, and CKD5 are poor prognostic factors. Overall, 5-10% of patients develop B-cell lymphoma within 5 years of CV diagnosis, and 5% of patients with SS develop lymphoma. Despite diagnostic uncertainty, early immunosuppression before bacterial translocation and perforation may have been life-saving in her case.

Disclosures:
Jennifer Claytor, MD1, David Greenwald, MD2. P1650 - A Fatal Case of Cryoglobulinemic Vasculitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai Hospital, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Cryoglobulinemic Vasculitis (CV) is rare; prior to effective antivirals, 90% of cases co-occurred with Hepatitis C. In patients with Sjogren’s Syndrome (SS), lymphoma, or other rheumatologic disorders, CV can be an unusual cause of catastrophic gastrointestinal (GI) hemorrhage and ischemia.
Case Description/Methods: A 74-year-old woman with SS on steroids and chronic kidney disease (CKD) IV due to cryoglobulinemic glomerulonephritis (GN) presented with melena and abdominal distension. She had mild renal and hepatic injury; negative Hepatitis B and C studies; and no further melena in the hospital. CT showed a single loop of thickened small bowel, 2 hepatic masses, and a pericardial effusion, “highly concerning for lymphoma or other malignancy”. She was transferred for possible balloon enteroscopy.
Push enteroscopy showed a violaceous, necrotic, obstructing mass and severe duodenitis in D3-4, favoring GI lymphoma over atypical infection and ischemia. Pathology showed acute on chronic duodenitis with sloughed epithelium. Flow cytometry was mostly acellular, with no clear evidence of lymphoma. Not having started outpatient rituximab and now acutely ill, she had anuric renal failure. ANA was strongly positive; RF, elevated, and C4, undetectable. Serum cryoglobulins were negative. She developed acute hematochezia.
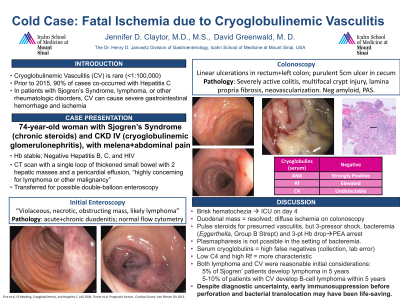
EGD and colonoscopy were performed. The violaceous duodenal mass had disappeared, although granularity and erythema persisted. There were large ulcers in the rectum; a long, linear ulceration in the descending colon; and a purulent, ulcer bed >4cm in diameter obscuring the cecum. Pathology showed severely active nonspecific colitis, multifocal crypt injury, and neovascularization. Pulse steroids were started for presumed GI CV. On day 4, she developed with dual-pressor shock and had bacteremia, precluding plasmapheresis. Repeat CT showed infarctions of the spleen, kidneys, and liver. With worsening septic shock, she experienced PEA arrest and died.
Discussion: GI CV is rare and potentially fatal. Serum cryoglobulin testing is unreliable, with many false negatives due to incubation and collection error; low C4 and high RF are more typical. Older age, pulmonary or GI involvement, and CKD5 are poor prognostic factors. Overall, 5-10% of patients develop B-cell lymphoma within 5 years of CV diagnosis, and 5% of patients with SS develop lymphoma. Despite diagnostic uncertainty, early immunosuppression before bacterial translocation and perforation may have been life-saving in her case.

Figure: Cecal Ulceration
Disclosures:
Jennifer Claytor indicated no relevant financial relationships.
David Greenwald indicated no relevant financial relationships.
Jennifer Claytor, MD1, David Greenwald, MD2. P1650 - A Fatal Case of Cryoglobulinemic Vasculitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
