Monday Poster Session
Category: Colon
P1656 - Neither One nor the Other: Lymphocytic Enterocolitis as the Cause of Chronic Diarrhea
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Ricardo L. López-Valle, MD
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Ricardo L.. López-Valle, MD, Miguel J.. Anzalota-Del Toro, MD, José Martin-Ortiz, MD, FACG
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Chronic diarrhea is a non-specific complaint that is often brought up by patients. When evaluating for causes of chronic diarrhea, microscopic colitis is one condition that should always be considered. In the case below we describe how a previously established diagnosis had to be questioned to achieve proper patient care.
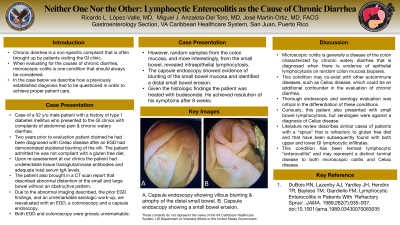
Case Description/Methods: 52 y/o male patient with history of type 1 diabetes mellitus who presented to the GI clinics with complaints of abdominal pain & chronic watery diarrhea. Two years prior to evaluation patient had been diagnosed with celiac disease after an EGD had demonstrated duodenal blunting of the villi. However, upon re-assessment at clinics patient had undetectable tissue transglutaminase antibodies and adequate total serum IgA levels. Patient admitted he was not compliant with a gluten free diet. Patient also brought a CT scan that demonstrated abnormal distention of the small and large bowel without an obstructive pattern. Due to abnormal imaging, prior EGD findings, and unremarkable serologic work-up the patient underwent an EGD, a colonoscopy, and a capsule endoscopy for further elucidation. Both EGD and colonoscopy were grossly unremarkable, but random samples of the colon mucosa, and more interestingly, from the small bowel, revealed intraepithelial lymphocytosis. Capsule endoscopy described blunting of the small bowel mucosa and identified a distal small bowel erosion. Given histologic findings patient was treated with budesonide and achieved complete resolution of his symptoms.
Discussion: Microscopic colitis is generally a disease of the colon characterized by chronic watery diarrhea that is diagnosed when there is evidence of epithelial lymphocytosis on random colon mucosa biopsies. This condition may co-exist with other auto-immune diseases, such as celiac disease, which could be an additional confounder in the evaluation of chronic diarrheas, as was the case in this patient. Thorough endoscopic and serology evaluation was critical in the differentiation of these conditions. Curiously, this patient also presented with small bowel lymphocytosis, but serologies went against a diagnosis of celiac disease. Literature review describes similar cases of patients with a sprue that is refractory to gluten free diet and that have been subsequently found with both upper and lower GI lymphocytic infiltrates. This condition has been termed lymphocytic “enterocolitis” and may represent a distinct intestinal disease to both microscopic colitis and celiac disease.
Disclosures:
Ricardo L.. López-Valle, MD, Miguel J.. Anzalota-Del Toro, MD, José Martin-Ortiz, MD, FACG. P1656 - Neither One nor the Other: Lymphocytic Enterocolitis as the Cause of Chronic Diarrhea, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Chronic diarrhea is a non-specific complaint that is often brought up by patients. When evaluating for causes of chronic diarrhea, microscopic colitis is one condition that should always be considered. In the case below we describe how a previously established diagnosis had to be questioned to achieve proper patient care.
Case Description/Methods: 52 y/o male patient with history of type 1 diabetes mellitus who presented to the GI clinics with complaints of abdominal pain & chronic watery diarrhea. Two years prior to evaluation patient had been diagnosed with celiac disease after an EGD had demonstrated duodenal blunting of the villi. However, upon re-assessment at clinics patient had undetectable tissue transglutaminase antibodies and adequate total serum IgA levels. Patient admitted he was not compliant with a gluten free diet. Patient also brought a CT scan that demonstrated abnormal distention of the small and large bowel without an obstructive pattern. Due to abnormal imaging, prior EGD findings, and unremarkable serologic work-up the patient underwent an EGD, a colonoscopy, and a capsule endoscopy for further elucidation. Both EGD and colonoscopy were grossly unremarkable, but random samples of the colon mucosa, and more interestingly, from the small bowel, revealed intraepithelial lymphocytosis. Capsule endoscopy described blunting of the small bowel mucosa and identified a distal small bowel erosion. Given histologic findings patient was treated with budesonide and achieved complete resolution of his symptoms.
Discussion: Microscopic colitis is generally a disease of the colon characterized by chronic watery diarrhea that is diagnosed when there is evidence of epithelial lymphocytosis on random colon mucosa biopsies. This condition may co-exist with other auto-immune diseases, such as celiac disease, which could be an additional confounder in the evaluation of chronic diarrheas, as was the case in this patient. Thorough endoscopic and serology evaluation was critical in the differentiation of these conditions. Curiously, this patient also presented with small bowel lymphocytosis, but serologies went against a diagnosis of celiac disease. Literature review describes similar cases of patients with a sprue that is refractory to gluten free diet and that have been subsequently found with both upper and lower GI lymphocytic infiltrates. This condition has been termed lymphocytic “enterocolitis” and may represent a distinct intestinal disease to both microscopic colitis and celiac disease.
Disclosures:
Ricardo López-Valle indicated no relevant financial relationships.
Miguel Anzalota-Del Toro indicated no relevant financial relationships.
José Martin-Ortiz indicated no relevant financial relationships.
Ricardo L.. López-Valle, MD, Miguel J.. Anzalota-Del Toro, MD, José Martin-Ortiz, MD, FACG. P1656 - Neither One nor the Other: Lymphocytic Enterocolitis as the Cause of Chronic Diarrhea, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
