Monday Poster Session
Category: Colon
P1659 - The Cancer Diaspora: A Rare Case of Pseudomyxoma Peritonei of Appendiceal Origin
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Lefika Bathobakae, MD, MPH
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Lefika Bathobakae, MD, MPH1, Sacide S. Ozgur, MD1, Mohita Jariwala, BA2, Jaydev Kesrani, MD1, Shajla Ajas, MD1, Mehandar Kumar, MD1
1St. Joseph's University Medical Center, Paterson, NJ; 2Rowan University School of Osteopathic Medicine, Paterson, NJ
Introduction: Pseudomyxoma peritonei (PMP) is a rare neoplasm characterized by the dissemination of mucous ascites within the peritoneal cavity from a ruptured appendiceal or ovarian neoplasm. Herein, we present a rare case of PMP in a female patient with a three-month history of progressive abdominal distension.
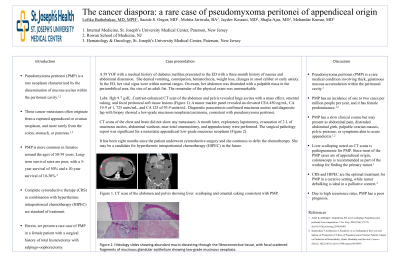
Case Description/Methods: A 59-year-old female with a history of diabetes mellitus presented to the ED with a three-month history of nausea and abdominal distension. She denied vomiting, constipation, hematochezia, weight loss, changes in stool caliber or early satiety. In the ED, her vitals were within normal. On exam, her abdomen was distended with a palpable mass in the periumbilical area, the size of an adult fist. The remainder of the physical exam was unremarkable. Labs: Hgb 9.7 g/dL. CT scan of the abdomen and pelvis with contrast revealed large ascites with a mass effect, omental caking, and focal peritoneal soft tissue lesions. A tumor marker panel revealed an elevated CEA 450 ng/ml, CA 19–9 of 1725 units/ml, and CA 125 of 93.9 units/ml. Diagnostic paracentesis confirmed mucinous ascites and diagnostic lap with biopsy showed a low-grade mucinous neoplasia/carcinoma, consistent with pseudomyxoma peritonei. CT scans of the chest and brain did not show any metastases. A month later, exploratory laparotomy, evacuation of 2 L of mucinous ascites, abdominal washout, near-total omentectomy, and appendectomy were performed. The surgical pathology report was significant for a metastatic appendiceal low-grade mucinous neoplasm. Patient may be a candidate for hyperthermic intraperitoneal chemotherapy (HIPEC) in the future.
Discussion: Pseudomyxoma peritonei (PMP) is a rare medical condition involving thick, gelatinous mucous accumulation within the peritoneal cavity. PMP has an incidence of one to two cases per million people per year, and it has female predominance. PMP has a slow clinical course but may present as abdominal pain, distended abdominal girth, palpable ovarian masses, pelvic pressure, or symptoms akin to acute appendicitis. Liver scalloping noted on CT scans is pathognomonic for PMP. Since most of the PMP cases are of appendiceal origin, a colonoscopy is recommended as part of the workup for finding the primary tumor. CRS and HIPEC are the optimal treatment for PMP in a curative setting, while tumor debulking is ideal in palliative care. Due to high recurrence rates, PMP has a poor prognosis.

Disclosures:
Lefika Bathobakae, MD, MPH1, Sacide S. Ozgur, MD1, Mohita Jariwala, BA2, Jaydev Kesrani, MD1, Shajla Ajas, MD1, Mehandar Kumar, MD1. P1659 - The Cancer Diaspora: A Rare Case of Pseudomyxoma Peritonei of Appendiceal Origin, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1St. Joseph's University Medical Center, Paterson, NJ; 2Rowan University School of Osteopathic Medicine, Paterson, NJ
Introduction: Pseudomyxoma peritonei (PMP) is a rare neoplasm characterized by the dissemination of mucous ascites within the peritoneal cavity from a ruptured appendiceal or ovarian neoplasm. Herein, we present a rare case of PMP in a female patient with a three-month history of progressive abdominal distension.
Case Description/Methods: A 59-year-old female with a history of diabetes mellitus presented to the ED with a three-month history of nausea and abdominal distension. She denied vomiting, constipation, hematochezia, weight loss, changes in stool caliber or early satiety. In the ED, her vitals were within normal. On exam, her abdomen was distended with a palpable mass in the periumbilical area, the size of an adult fist. The remainder of the physical exam was unremarkable. Labs: Hgb 9.7 g/dL. CT scan of the abdomen and pelvis with contrast revealed large ascites with a mass effect, omental caking, and focal peritoneal soft tissue lesions. A tumor marker panel revealed an elevated CEA 450 ng/ml, CA 19–9 of 1725 units/ml, and CA 125 of 93.9 units/ml. Diagnostic paracentesis confirmed mucinous ascites and diagnostic lap with biopsy showed a low-grade mucinous neoplasia/carcinoma, consistent with pseudomyxoma peritonei. CT scans of the chest and brain did not show any metastases. A month later, exploratory laparotomy, evacuation of 2 L of mucinous ascites, abdominal washout, near-total omentectomy, and appendectomy were performed. The surgical pathology report was significant for a metastatic appendiceal low-grade mucinous neoplasm. Patient may be a candidate for hyperthermic intraperitoneal chemotherapy (HIPEC) in the future.
Discussion: Pseudomyxoma peritonei (PMP) is a rare medical condition involving thick, gelatinous mucous accumulation within the peritoneal cavity. PMP has an incidence of one to two cases per million people per year, and it has female predominance. PMP has a slow clinical course but may present as abdominal pain, distended abdominal girth, palpable ovarian masses, pelvic pressure, or symptoms akin to acute appendicitis. Liver scalloping noted on CT scans is pathognomonic for PMP. Since most of the PMP cases are of appendiceal origin, a colonoscopy is recommended as part of the workup for finding the primary tumor. CRS and HIPEC are the optimal treatment for PMP in a curative setting, while tumor debulking is ideal in palliative care. Due to high recurrence rates, PMP has a poor prognosis.

Figure: Figure 1. A CT scan of the abdomen and pelvis showed liver scalloping (red arrows) and omental caking (black arrows) consistent with Pseudomyxoma peritonei.
Disclosures:
Lefika Bathobakae indicated no relevant financial relationships.
Sacide Ozgur indicated no relevant financial relationships.
Mohita Jariwala indicated no relevant financial relationships.
Jaydev Kesrani indicated no relevant financial relationships.
Shajla Ajas indicated no relevant financial relationships.
Mehandar Kumar indicated no relevant financial relationships.
Lefika Bathobakae, MD, MPH1, Sacide S. Ozgur, MD1, Mohita Jariwala, BA2, Jaydev Kesrani, MD1, Shajla Ajas, MD1, Mehandar Kumar, MD1. P1659 - The Cancer Diaspora: A Rare Case of Pseudomyxoma Peritonei of Appendiceal Origin, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
