Monday Poster Session
Category: Colon
P1673 - Unmasking the Hidden: Mpox-Induced Proctocolitis Disguised as Painful Hemorrhoids
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sobaan Taj, MD
Hackensack Meridian Jersey Shore University Medical Center
Neptune, NJ
Presenting Author(s)
Sobaan Taj, MD1, Zaka Ul Haq, MD2, Henna Pervaiz, MD3, Harshavardhan Sanekommu, MD4, Saira Chaughtai, MD4
1Hackensack Meridian Jersey Shore University Medical Center, Neptune, NJ; 2Raritan Bay Medical Center, Edison, NJ; 3SUNY Downstate Medical Center, Brooklyn, NJ; 4Jersey Shore University Medical Center, Woodbridge, NJ
Introduction: Monkeypox, an orthopoxvirus, is primarily a skin disease but can cause systemic symptoms like proctitis and severe rectal pain. Diagnosis is challenging as these symptoms are prevalent in many other anal and rectal disorders, potentially leading to delayed treatment. This report describes a case of a young male who mistook these symptoms for his known hemorrhoids, thus delaying his medical consultation.
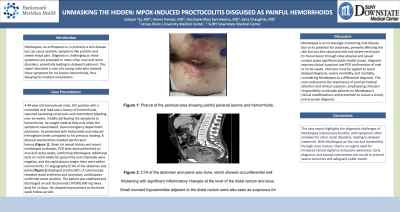
Case Description/Methods: A 40-year-old homosexual male, HIV positive with a controlled viral load and a history of hemorrhoids, reported escalating rectal pain and intermittent bleeding over six weeks. Initially attributing the symptoms to hemorrhoids, he sought medical help only when the symptoms exacerbated. Upon emergency department admission, he presented with tachycardia and reduced hemoglobin levels compared to his previous reading. A physical examination revealed painful anal lesions (Figure 1). Given his sexual history and recent monkeypox outbreaks, PCR tests were performed on anal and rectal swabs, confirming Monkeypox. Additional tests on rectal swabs for gonorrhea and chlamydia were negative, and the rapid plasma reagin titers were within normal limits. CT angiography (CTA) of the abdomen and pelvis (Figure 2) displayed proctocolitis. A colonoscopy revealed rectal erythema and ulceration, and biopsies confirmed acute proctitis. The patient was stabilized and discharged on oral Tecovirimat (TPOXX) 600 mg twice daily for 14 days. He showed improvement at the three-week follow-up visit.
Discussion: Monkeypox is an increasingly concerning viral disease due to its potential for outbreaks, primarily affecting the skin but can also cause proctitis and severe rectal pain. Its transmission through close physical and sexual contact poses significant public health issues. Diagnosis requires clinical suspicion and PCR confirmation of anal or rectal swabs. Clinicians must be vigilant to avoid delayed diagnosis, severe morbidity, and mortality, considering Monkeypox as a differential diagnosis. This case underscores the importance of prompt medical attention and clinical suspicion, emphasizing clinicians' responsibility to educate patients on Monkeypox's clinical manifestations and prevention to ensure a timely and accurate diagnosis.

Disclosures:
Sobaan Taj, MD1, Zaka Ul Haq, MD2, Henna Pervaiz, MD3, Harshavardhan Sanekommu, MD4, Saira Chaughtai, MD4. P1673 - Unmasking the Hidden: Mpox-Induced Proctocolitis Disguised as Painful Hemorrhoids, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Hackensack Meridian Jersey Shore University Medical Center, Neptune, NJ; 2Raritan Bay Medical Center, Edison, NJ; 3SUNY Downstate Medical Center, Brooklyn, NJ; 4Jersey Shore University Medical Center, Woodbridge, NJ
Introduction: Monkeypox, an orthopoxvirus, is primarily a skin disease but can cause systemic symptoms like proctitis and severe rectal pain. Diagnosis is challenging as these symptoms are prevalent in many other anal and rectal disorders, potentially leading to delayed treatment. This report describes a case of a young male who mistook these symptoms for his known hemorrhoids, thus delaying his medical consultation.
Case Description/Methods: A 40-year-old homosexual male, HIV positive with a controlled viral load and a history of hemorrhoids, reported escalating rectal pain and intermittent bleeding over six weeks. Initially attributing the symptoms to hemorrhoids, he sought medical help only when the symptoms exacerbated. Upon emergency department admission, he presented with tachycardia and reduced hemoglobin levels compared to his previous reading. A physical examination revealed painful anal lesions (Figure 1). Given his sexual history and recent monkeypox outbreaks, PCR tests were performed on anal and rectal swabs, confirming Monkeypox. Additional tests on rectal swabs for gonorrhea and chlamydia were negative, and the rapid plasma reagin titers were within normal limits. CT angiography (CTA) of the abdomen and pelvis (Figure 2) displayed proctocolitis. A colonoscopy revealed rectal erythema and ulceration, and biopsies confirmed acute proctitis. The patient was stabilized and discharged on oral Tecovirimat (TPOXX) 600 mg twice daily for 14 days. He showed improvement at the three-week follow-up visit.
Discussion: Monkeypox is an increasingly concerning viral disease due to its potential for outbreaks, primarily affecting the skin but can also cause proctitis and severe rectal pain. Its transmission through close physical and sexual contact poses significant public health issues. Diagnosis requires clinical suspicion and PCR confirmation of anal or rectal swabs. Clinicians must be vigilant to avoid delayed diagnosis, severe morbidity, and mortality, considering Monkeypox as a differential diagnosis. This case underscores the importance of prompt medical attention and clinical suspicion, emphasizing clinicians' responsibility to educate patients on Monkeypox's clinical manifestations and prevention to ensure a timely and accurate diagnosis.

Figure: Captions are mentioned in the Figure.
Disclosures:
Sobaan Taj indicated no relevant financial relationships.
Zaka Ul Haq indicated no relevant financial relationships.
Henna Pervaiz indicated no relevant financial relationships.
Harshavardhan Sanekommu indicated no relevant financial relationships.
Saira Chaughtai indicated no relevant financial relationships.
Sobaan Taj, MD1, Zaka Ul Haq, MD2, Henna Pervaiz, MD3, Harshavardhan Sanekommu, MD4, Saira Chaughtai, MD4. P1673 - Unmasking the Hidden: Mpox-Induced Proctocolitis Disguised as Painful Hemorrhoids, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

