Monday Poster Session
Category: Colon
P1706 - Hematochezia Discovered to Be Anorectal Amelanotic Melanoma
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Gnanashree Dharmarpandi, MD
Texas Tech University Health Sciences Center
Amarillo, TX
Presenting Author(s)
Gnanashree Dharmarpandi, MD1, Waqas Rasheed, MD1, Muhammad Anil, MD2, Shahana ishfaque, MBBS3, Muhammad Anees, MD1, Sarah Naveed. Qureshi, MBBS4
1Texas Tech University Health Sciences Center, Amarillo, TX; 2Beaumont Hospital, Dearborn, MI; 3Punjab Medical College, Faisalabad, Pakistan, Dearborn, MI; 4CMH Multan Institute of Medical Sciences, Multan, Pakistan, Beaumont, TX
Introduction: Most anorectal tumors are either adenocarcinoma or squamous cell carcinoma but there are other rare entities including lymphoma, melanoma, hemangioma, or sarcoma. Anorectal melanoma (AM) is very uncommon, usually presenting at 6th decade of life in females, and comprises only 1-2% of gastrointestinal malignancies. We present an interesting case of anorectal melanoma found in a patient with hematochezia.
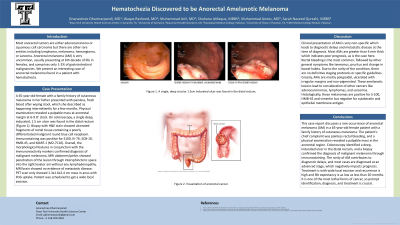
Case Description/Methods: A 65-year-old-female with a family history of cutaneous melanoma in her father presented with painless, fresh blood after wiping stool, which she described as happening intermittently for a few months. Physical examination revealed a palpable mass at anorectal margin at 6-9 O' clock. On colonoscopy, a single deep, indurated, 1.5 cm ulcer was found in the distal rectum (Figure 1). Biopsy with H&E stain showed ulcerated fragments of rectal tissue containing a poorly differentiated malignant round blue cell neoplasm. Immunostaining was positive for S100, Ki-76, SOX-10, HMB-45, and MART-1 (M2-7C10). Overall, the morphological features in conjunction with the immunoreactivity markers confirmed diagnosis of malignant melanoma. MRI abdomen/pelvis showed penetration of the lesion through intersphincteric space into the right levator ani without any lymphadenopathy. MRI brain showed no evidence of metastatic disease. PET scan only showed 1.3x1.6x2.4 cm mass in anus with FDG uptake. Patient was scheduled to get a wide local excision.
Discussion: Clinical presentation of AM is very non-specific which leads to diagnostic delays and metastatic disease at the time of diagnosis. Most AMs are greater than 4 mm thick which indicates poor prognosis, as is the case here. Rectal bleeding is the most common, followed by other general symptoms like tenesmus, pruritus and change in bowel habits. Due to the rarity of the condition, there are no definitive staging protocols or specific guidelines. Grossly, AMs are mostly polypoidal, ulcerated with irregular margins and non-pigmented. These amelanotic lesions lead to consideration of other cancers like adenocarcinomas, lymphomas, and sarcomas. Histologically, these melanomas are positive for S-100, HMB-45 and vimentin but negative for cytokeratin and epithelial membrane antigen. Treatment is with wide local excision and recurrence is high and life expectancy is as low as less than 20 months. It is one of the most lethal forms of cancer, so prompt identification, diagnosis, and treatment is crucial.

Disclosures:
Gnanashree Dharmarpandi, MD1, Waqas Rasheed, MD1, Muhammad Anil, MD2, Shahana ishfaque, MBBS3, Muhammad Anees, MD1, Sarah Naveed. Qureshi, MBBS4. P1706 - Hematochezia Discovered to Be Anorectal Amelanotic Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, Amarillo, TX; 2Beaumont Hospital, Dearborn, MI; 3Punjab Medical College, Faisalabad, Pakistan, Dearborn, MI; 4CMH Multan Institute of Medical Sciences, Multan, Pakistan, Beaumont, TX
Introduction: Most anorectal tumors are either adenocarcinoma or squamous cell carcinoma but there are other rare entities including lymphoma, melanoma, hemangioma, or sarcoma. Anorectal melanoma (AM) is very uncommon, usually presenting at 6th decade of life in females, and comprises only 1-2% of gastrointestinal malignancies. We present an interesting case of anorectal melanoma found in a patient with hematochezia.
Case Description/Methods: A 65-year-old-female with a family history of cutaneous melanoma in her father presented with painless, fresh blood after wiping stool, which she described as happening intermittently for a few months. Physical examination revealed a palpable mass at anorectal margin at 6-9 O' clock. On colonoscopy, a single deep, indurated, 1.5 cm ulcer was found in the distal rectum (Figure 1). Biopsy with H&E stain showed ulcerated fragments of rectal tissue containing a poorly differentiated malignant round blue cell neoplasm. Immunostaining was positive for S100, Ki-76, SOX-10, HMB-45, and MART-1 (M2-7C10). Overall, the morphological features in conjunction with the immunoreactivity markers confirmed diagnosis of malignant melanoma. MRI abdomen/pelvis showed penetration of the lesion through intersphincteric space into the right levator ani without any lymphadenopathy. MRI brain showed no evidence of metastatic disease. PET scan only showed 1.3x1.6x2.4 cm mass in anus with FDG uptake. Patient was scheduled to get a wide local excision.
Discussion: Clinical presentation of AM is very non-specific which leads to diagnostic delays and metastatic disease at the time of diagnosis. Most AMs are greater than 4 mm thick which indicates poor prognosis, as is the case here. Rectal bleeding is the most common, followed by other general symptoms like tenesmus, pruritus and change in bowel habits. Due to the rarity of the condition, there are no definitive staging protocols or specific guidelines. Grossly, AMs are mostly polypoidal, ulcerated with irregular margins and non-pigmented. These amelanotic lesions lead to consideration of other cancers like adenocarcinomas, lymphomas, and sarcomas. Histologically, these melanomas are positive for S-100, HMB-45 and vimentin but negative for cytokeratin and epithelial membrane antigen. Treatment is with wide local excision and recurrence is high and life expectancy is as low as less than 20 months. It is one of the most lethal forms of cancer, so prompt identification, diagnosis, and treatment is crucial.

Figure: Figure 1. Anorectal ulceration from anorectal amelanotic melanoma
Disclosures:
Gnanashree Dharmarpandi indicated no relevant financial relationships.
Waqas Rasheed indicated no relevant financial relationships.
Muhammad Anil indicated no relevant financial relationships.
Shahana ishfaque indicated no relevant financial relationships.
Muhammad Anees indicated no relevant financial relationships.
Sarah Qureshi indicated no relevant financial relationships.
Gnanashree Dharmarpandi, MD1, Waqas Rasheed, MD1, Muhammad Anil, MD2, Shahana ishfaque, MBBS3, Muhammad Anees, MD1, Sarah Naveed. Qureshi, MBBS4. P1706 - Hematochezia Discovered to Be Anorectal Amelanotic Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
