Monday Poster Session
Category: Colon
P1709 - It’s Never Too Late to Develop Immune Checkpoint Inhibitor Enterocolitis: A Case Report
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Danyal O. Imam, MD
Riverside University Health System
Moreno Valley, CA
Presenting Author(s)
Danyal O. Imam, MD1, Brook Yirgu, MS2, Kristen Anderson, MD, PhD1, Ronaldo Gnass, MD1, Bing Wang, MD1, Steve Serrao, MD, PhD1
1Riverside University Health System, Moreno Valley, CA; 2University of California Riverside School of Medicine, Riverside, CA
Introduction: Immune Checkpoint Inhibitors (ICI) are monoclonal antibodies targeting cellular pathways involved in T-cell mediated immune response and are used in the treatment of various types of cancer. A common side-effect is diarrhea due to colitis. This usually occurs 1-2 months after the initiation of therapy but can occur at any point during treatment. We present a case of late onset immune mediated colitis (IMC).
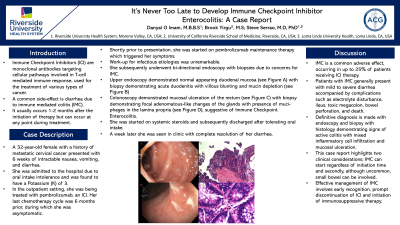
Case Description/Methods: A 32-year-old female with a history of metastatic cervical cancer presented with 6 weeks of intractable nausea, vomiting, diarrhea, and hypokalemia. She was being treated with a chemotherapy regimen that included pembrolizumab, an ICI. Her last chemotherapy cycle was 6 months ago during which she was asymptomatic. She was recently started on pembrolizumab maintenance therapy, which triggered her symptoms. Workup was negative for infectious etiologies. She underwent esophagogastroduodenoscopy (EGD) and colonoscopy due to suspicion of IMC. EGD demonstrated normal appearing duodenal mucosa (figure A) but biopsy showed duodenitis with villous blunting and mucin depletion (figure B). Colonoscopy revealed mucosal ulceration in the rectum (figure C) and biopsy showed chronic active proctitis with focal adenomatous-like changes of the glands and presence of muciphages in the lamina propria, consistent with IMC (figure D). She was started on systemic steroids and subsequently discharged after tolerating oral intake. A week later she was seen in clinic with complete resolution of her diarrhea.
Discussion: IMC is a common adverse effect, occurring in up to 25% of patients receiving ICI therapy. The prevailing hypothesis is that unchecked T-cell activation from ICI leads to induction of autoimmunity resulting in colitis. Patients with IMC generally present with mild to severe diarrhea accompanied by complications such as electrolyte disturbance, ileus, toxic megacolon, bowel perforation, and death. Definitive diagnosis is made with endoscopy and biopsy. Histology typically demonstrates signs of active colitis with mixed inflammatory cell infiltration and mucosal ulceration. This case report highlights two clinical considerations; IMC can start regardless of initiation time and secondly, although uncommon, small bowel can be involved. Effective management of IMC involves early recognition, prompt discontinuation of ICI and initiation of immunosuppressive therapy.

Disclosures:
Danyal O. Imam, MD1, Brook Yirgu, MS2, Kristen Anderson, MD, PhD1, Ronaldo Gnass, MD1, Bing Wang, MD1, Steve Serrao, MD, PhD1. P1709 - It’s Never Too Late to Develop Immune Checkpoint Inhibitor Enterocolitis: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Riverside University Health System, Moreno Valley, CA; 2University of California Riverside School of Medicine, Riverside, CA
Introduction: Immune Checkpoint Inhibitors (ICI) are monoclonal antibodies targeting cellular pathways involved in T-cell mediated immune response and are used in the treatment of various types of cancer. A common side-effect is diarrhea due to colitis. This usually occurs 1-2 months after the initiation of therapy but can occur at any point during treatment. We present a case of late onset immune mediated colitis (IMC).
Case Description/Methods: A 32-year-old female with a history of metastatic cervical cancer presented with 6 weeks of intractable nausea, vomiting, diarrhea, and hypokalemia. She was being treated with a chemotherapy regimen that included pembrolizumab, an ICI. Her last chemotherapy cycle was 6 months ago during which she was asymptomatic. She was recently started on pembrolizumab maintenance therapy, which triggered her symptoms. Workup was negative for infectious etiologies. She underwent esophagogastroduodenoscopy (EGD) and colonoscopy due to suspicion of IMC. EGD demonstrated normal appearing duodenal mucosa (figure A) but biopsy showed duodenitis with villous blunting and mucin depletion (figure B). Colonoscopy revealed mucosal ulceration in the rectum (figure C) and biopsy showed chronic active proctitis with focal adenomatous-like changes of the glands and presence of muciphages in the lamina propria, consistent with IMC (figure D). She was started on systemic steroids and subsequently discharged after tolerating oral intake. A week later she was seen in clinic with complete resolution of her diarrhea.
Discussion: IMC is a common adverse effect, occurring in up to 25% of patients receiving ICI therapy. The prevailing hypothesis is that unchecked T-cell activation from ICI leads to induction of autoimmunity resulting in colitis. Patients with IMC generally present with mild to severe diarrhea accompanied by complications such as electrolyte disturbance, ileus, toxic megacolon, bowel perforation, and death. Definitive diagnosis is made with endoscopy and biopsy. Histology typically demonstrates signs of active colitis with mixed inflammatory cell infiltration and mucosal ulceration. This case report highlights two clinical considerations; IMC can start regardless of initiation time and secondly, although uncommon, small bowel can be involved. Effective management of IMC involves early recognition, prompt discontinuation of ICI and initiation of immunosuppressive therapy.

Figure: A: Normal-appearing mucosa of 2nd portion of duodenum; B: Duodenitis with villous blunting; C: Ulcerated mucosa of rectum; D: Chronic active Proctitis with presence of muciphages in the lamina propria
Disclosures:
Danyal Imam indicated no relevant financial relationships.
Brook Yirgu indicated no relevant financial relationships.
Kristen Anderson indicated no relevant financial relationships.
Ronaldo Gnass indicated no relevant financial relationships.
Bing Wang indicated no relevant financial relationships.
Steve Serrao indicated no relevant financial relationships.
Danyal O. Imam, MD1, Brook Yirgu, MS2, Kristen Anderson, MD, PhD1, Ronaldo Gnass, MD1, Bing Wang, MD1, Steve Serrao, MD, PhD1. P1709 - It’s Never Too Late to Develop Immune Checkpoint Inhibitor Enterocolitis: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
