Monday Poster Session
Category: Colon
P1732 - A Rare Case of Stercoral Colitis Leading to Colonic Wall Ischemia at the Splenic Flexure
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Megan B. Ghai, MD, MPH, MA
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Megan B. Ghai, MD, MPH, MA1, Kelly Zucker, DO2, Natasha Narang, DO1, Jesus Sandoval Macias, MD1, Teresa Diaz, MD3, Camron Kiafar, DO, FACG4
1University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona, Phoenix, AZ; 3VA Phoenix Medical Center, Phoenix, AZ; 4Phoenix VA Medical Center, Phoenix, AZ
Introduction: Stercoral colitis is a rare inflammatory condition in which stool impaction leads to increased intraluminal pressure that can result in colonic wall ischemia, ulceration, and perforation. It is associated with a mortality rate as high as 60%, thus timely management is essential. Chronic constipation is one of the biggest risk factors of stercoral colitis and it is most commonly seen at the level of the rectum. Presented is a rare case of stercoral colitis found at the splenic flexure.
Case Description/Methods: A 73-year-old male with a past medical history of type two diabetes mellitus, atrial fibrillation, and prostate cancer presented to the hospital with two weeks of abdominal pain and constipation, progressing to 3 days of obstipation. He had no prior history of gastrointestinal conditions and had an unremarkable colonoscopy two years prior. On admission his vitals, physical exam, and blood work were unremarkable. Computed tomography (CT) of the abdomen with intravenous contrast revealed a large stool burden at the splenic flexure with a transition point in the descending colon concerning for partial obstruction (Figure 1a). Flexible sigmoidoscopy revealed a large formed stool at the splenic flexure with surrounding friable mucosa concerning for ischemic changes. Forceps and water jet were used to break up the stool burden. Two days later, repeat CT demonstrated new wall thickening and luminal narrowing in the descending colon concerning for reactive ischemia at the site of the prior stool impaction (Figure 1b). The patient clinically improved with scheduled bowel care and was discharged on a low residue diet. Six weeks later, repeat CT revealed loss of haustral markings reflecting late sequelae of ischemia, though the patient remained clinically stable (Figure 1c).
Discussion: This is an unusual case of stercoral colitis at the level of the splenic flexure leading to pressure necrosis and bowel ischemia. While stercoral colitis is often seen at level of the rectum, there are few reports of stercoral colitis with the sequelae of ischemia seen at the splenic flexure. It is hypothesized that the narrowing and partial volvulus of the descending colon led to upstream stool burden at the splenic flexure. These findings can also be secondary to an underlying mass, adhesions, stricture, or diverticulitis which is why follow up imaging was required. This case demonstrates the importance of adequate bowel care to prevent serious complications of constipation.

Disclosures:
Megan B. Ghai, MD, MPH, MA1, Kelly Zucker, DO2, Natasha Narang, DO1, Jesus Sandoval Macias, MD1, Teresa Diaz, MD3, Camron Kiafar, DO, FACG4. P1732 - A Rare Case of Stercoral Colitis Leading to Colonic Wall Ischemia at the Splenic Flexure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona, Phoenix, AZ; 3VA Phoenix Medical Center, Phoenix, AZ; 4Phoenix VA Medical Center, Phoenix, AZ
Introduction: Stercoral colitis is a rare inflammatory condition in which stool impaction leads to increased intraluminal pressure that can result in colonic wall ischemia, ulceration, and perforation. It is associated with a mortality rate as high as 60%, thus timely management is essential. Chronic constipation is one of the biggest risk factors of stercoral colitis and it is most commonly seen at the level of the rectum. Presented is a rare case of stercoral colitis found at the splenic flexure.
Case Description/Methods: A 73-year-old male with a past medical history of type two diabetes mellitus, atrial fibrillation, and prostate cancer presented to the hospital with two weeks of abdominal pain and constipation, progressing to 3 days of obstipation. He had no prior history of gastrointestinal conditions and had an unremarkable colonoscopy two years prior. On admission his vitals, physical exam, and blood work were unremarkable. Computed tomography (CT) of the abdomen with intravenous contrast revealed a large stool burden at the splenic flexure with a transition point in the descending colon concerning for partial obstruction (Figure 1a). Flexible sigmoidoscopy revealed a large formed stool at the splenic flexure with surrounding friable mucosa concerning for ischemic changes. Forceps and water jet were used to break up the stool burden. Two days later, repeat CT demonstrated new wall thickening and luminal narrowing in the descending colon concerning for reactive ischemia at the site of the prior stool impaction (Figure 1b). The patient clinically improved with scheduled bowel care and was discharged on a low residue diet. Six weeks later, repeat CT revealed loss of haustral markings reflecting late sequelae of ischemia, though the patient remained clinically stable (Figure 1c).
Discussion: This is an unusual case of stercoral colitis at the level of the splenic flexure leading to pressure necrosis and bowel ischemia. While stercoral colitis is often seen at level of the rectum, there are few reports of stercoral colitis with the sequelae of ischemia seen at the splenic flexure. It is hypothesized that the narrowing and partial volvulus of the descending colon led to upstream stool burden at the splenic flexure. These findings can also be secondary to an underlying mass, adhesions, stricture, or diverticulitis which is why follow up imaging was required. This case demonstrates the importance of adequate bowel care to prevent serious complications of constipation.

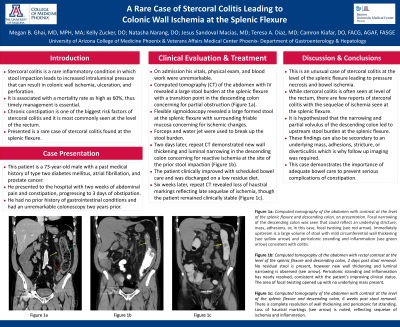
Figure: Figure 1a: Computed tomography of the abdomen with contrast at the level of the splenic flexure and descending colon, on presentation. Focal narrowing of the descending colon was seen that could reflect an underlying stricture, mass, adhesions, or, in this case, focal twisting (see red arrow). Immediately upstream is a large volume of stool with mild circumferential wall thickening (see yellow arrow) and pericolonic stranding and inflammation (see green arrow) consistent with colitis.
Figure 1b: Computed tomography of the abdomen with rectal contrast at the level of the splenic flexure and descending colon, 2 days post stool removal. No residual stool is present, however new wall thickening and luminal narrowing is observed (see arrow). Pericolonic stranding and inflammation has nearly resolved, consistent with the patient’s improving clinical status. The area of focal twisting opened up with no underlying mass present.
Figure 1c: Computed tomography of the abdomen with contrast at the level of the splenic flexure and descending colon, 6 weeks post stool removal. There is complete resolution of wall thickening and pericolonic fat stranding. Loss of haustral markings (see arrow) is noted, reflecting sequelae of ischemia and inflammation.
Figure 1b: Computed tomography of the abdomen with rectal contrast at the level of the splenic flexure and descending colon, 2 days post stool removal. No residual stool is present, however new wall thickening and luminal narrowing is observed (see arrow). Pericolonic stranding and inflammation has nearly resolved, consistent with the patient’s improving clinical status. The area of focal twisting opened up with no underlying mass present.
Figure 1c: Computed tomography of the abdomen with contrast at the level of the splenic flexure and descending colon, 6 weeks post stool removal. There is complete resolution of wall thickening and pericolonic fat stranding. Loss of haustral markings (see arrow) is noted, reflecting sequelae of ischemia and inflammation.
Disclosures:
Megan Ghai indicated no relevant financial relationships.
Kelly Zucker indicated no relevant financial relationships.
Natasha Narang indicated no relevant financial relationships.
Jesus Sandoval Macias indicated no relevant financial relationships.
Teresa Diaz indicated no relevant financial relationships.
Camron Kiafar indicated no relevant financial relationships.
Megan B. Ghai, MD, MPH, MA1, Kelly Zucker, DO2, Natasha Narang, DO1, Jesus Sandoval Macias, MD1, Teresa Diaz, MD3, Camron Kiafar, DO, FACG4. P1732 - A Rare Case of Stercoral Colitis Leading to Colonic Wall Ischemia at the Splenic Flexure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
