Monday Poster Session
Category: Colon
P1736 - Olmesartan-Induced Colonic Ischemia Causing a Mass-Like Lesion
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Robert Enders, MD, MS
California Pacific Medical Center
San Francisco, CA
Presenting Author(s)
Robert Enders, MD, MS1, Piyush Nathani, MBBS2, Ameer Hamza, MD3, Ajay Bansal, MD2, Mollie Jackson, DO2
1California Pacific Medical Center, San Francisco, CA; 2University of Kansas Health System, Kansas City, KS; 3University of Kansas Medical Center, Kansas City, KS
Introduction: Olmesartan, an ARB, has been associated with a sprue-like enteropathy that can cause chronic diarrhea. There are few reports of ischemic colitis (IC) resulting from olmesartan use, but never of a mass-like lesion.
Case Description/Methods: A 59 y/o woman with a PMH of celiac disease, GERD, gastric sleeve surgery, and HTN was admitted with acute abdominal pain and progressively worsening, nausea, vomiting, watery diarrhea, and reduced oral intake.
She was seen in the ED three days prior for similar symptoms. On admission, the patient reported up to 30 BMs per day with worsening abdominal pain. BP was 107/59 and HR was 118. Laboratory workup revealed Hgb of 11.5 g/dL and WBC count of 10.0 K/uL. Fecal leukocytes were positive but additional laboratory and stool workup was negative. A CT A/P with contrast from the ED visit showed mild wall thickening and adjacent fat stranding of the AC and the TC and numerous mildly enlarged mesenteric lymph nodes. Hemodynamic status improved with IV fluids and holding antihypertensives. Empiric antibiotics were started for presumed infectious diarrhea.
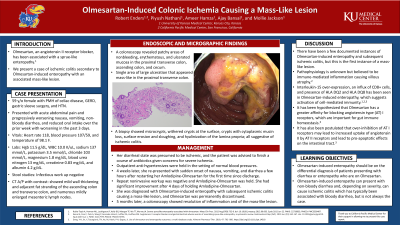
Colonoscopy revealed patchy areas of nonbleeding, erythematous, and ulcerated mucosa in the proximal TC, AC, and cecum; and a single area of large ulceration that appeared mass-like in the proximal TC. Biopsy results were suggestive of IC. Further infectious work up was negative. The patient was prescribed imodium and antibiotics for possible severe IC. Anti-hypertensives were temporarily held. A week later, she felt well and had normal BMs. The presumed etiology was viral gastroenteritis leading to IC.
Four weeks later, she presented again to the ED with sudden onset of nausea, vomiting, and diarrhea a few hours after restarting her amlodipine-olmesartan for the first time since discharge. She was admitted and repeat noninvasive workup of diarrhea was negative. Amlodipine-olmesartan was held and the patient noted symptomatic improvement. A diagnosis of olmesartan-induced enteropathy (OIE) and subsequent IC was made. Olmesartan was permanently discontinued.
Discussion: We describe a case of OIE that led to diagnostic confusion and multiple admissions. Our patient presented with severe diarrhea leading to hypotension, dehydration, and evidence of IC with a mass-like lesion seen on colonoscopy. During literature review, we found few documented instances of OIE and subsequent IC. This is the first instance of a mass-like lesion seen secondary to OIE causing IC.

Disclosures:
Robert Enders, MD, MS1, Piyush Nathani, MBBS2, Ameer Hamza, MD3, Ajay Bansal, MD2, Mollie Jackson, DO2. P1736 - Olmesartan-Induced Colonic Ischemia Causing a Mass-Like Lesion, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1California Pacific Medical Center, San Francisco, CA; 2University of Kansas Health System, Kansas City, KS; 3University of Kansas Medical Center, Kansas City, KS
Introduction: Olmesartan, an ARB, has been associated with a sprue-like enteropathy that can cause chronic diarrhea. There are few reports of ischemic colitis (IC) resulting from olmesartan use, but never of a mass-like lesion.
Case Description/Methods: A 59 y/o woman with a PMH of celiac disease, GERD, gastric sleeve surgery, and HTN was admitted with acute abdominal pain and progressively worsening, nausea, vomiting, watery diarrhea, and reduced oral intake.
She was seen in the ED three days prior for similar symptoms. On admission, the patient reported up to 30 BMs per day with worsening abdominal pain. BP was 107/59 and HR was 118. Laboratory workup revealed Hgb of 11.5 g/dL and WBC count of 10.0 K/uL. Fecal leukocytes were positive but additional laboratory and stool workup was negative. A CT A/P with contrast from the ED visit showed mild wall thickening and adjacent fat stranding of the AC and the TC and numerous mildly enlarged mesenteric lymph nodes. Hemodynamic status improved with IV fluids and holding antihypertensives. Empiric antibiotics were started for presumed infectious diarrhea.
Colonoscopy revealed patchy areas of nonbleeding, erythematous, and ulcerated mucosa in the proximal TC, AC, and cecum; and a single area of large ulceration that appeared mass-like in the proximal TC. Biopsy results were suggestive of IC. Further infectious work up was negative. The patient was prescribed imodium and antibiotics for possible severe IC. Anti-hypertensives were temporarily held. A week later, she felt well and had normal BMs. The presumed etiology was viral gastroenteritis leading to IC.
Four weeks later, she presented again to the ED with sudden onset of nausea, vomiting, and diarrhea a few hours after restarting her amlodipine-olmesartan for the first time since discharge. She was admitted and repeat noninvasive workup of diarrhea was negative. Amlodipine-olmesartan was held and the patient noted symptomatic improvement. A diagnosis of olmesartan-induced enteropathy (OIE) and subsequent IC was made. Olmesartan was permanently discontinued.
Discussion: We describe a case of OIE that led to diagnostic confusion and multiple admissions. Our patient presented with severe diarrhea leading to hypotension, dehydration, and evidence of IC with a mass-like lesion seen on colonoscopy. During literature review, we found few documented instances of OIE and subsequent IC. This is the first instance of a mass-like lesion seen secondary to OIE causing IC.

Figure: Proximal transverse colon with large ulceration that appeared mass-like.
Disclosures:
Robert Enders indicated no relevant financial relationships.
Piyush Nathani indicated no relevant financial relationships.
Ameer Hamza indicated no relevant financial relationships.
Ajay Bansal indicated no relevant financial relationships.
Mollie Jackson indicated no relevant financial relationships.
Robert Enders, MD, MS1, Piyush Nathani, MBBS2, Ameer Hamza, MD3, Ajay Bansal, MD2, Mollie Jackson, DO2. P1736 - Olmesartan-Induced Colonic Ischemia Causing a Mass-Like Lesion, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

