Monday Poster Session
Category: Colorectal Cancer Prevention
P1752 - Effect of the COVID-19 Pandemic on Colorectal Cancer Screening: An Analysis of Frequency, Modality, and Demographics
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Ann Kopera, DO
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Ann Kopera, DO1, Samantha Marshall, MD1, Harjit Singh, MD1, Sherry Gholami, MD1, Corinne O'Connor, MD1, Kavya Sanghavi, MPH2, Stephanie M. Woo, MD1, Nadim Haddad, MD1, Priyanka Kanth, MD, MS1
1MedStar Georgetown University Hospital, Washington, DC; 2MedStar Health Research Institute Center for Biostatistics, Washington, DC
Introduction: Colorectal cancer (CRC) is the second leading cause of cancer-related death in the United States. Data from the first year of the COVID-19 pandemic showed a decrease in screening colonoscopies that disproportionately affected African Americans. This study sought to determine the frequency, modality, and demographics of CRC screening two and a half years after the pandemic.
Methods: A retrospective chart review was conducted which included patients who completed colorectal cancer screening at MedStar Georgetown University Hospital from 9/1/2017-8/31/2022. March 1, 2020 was used as an inflection point. Patients were identified using CPT codes for screening colonoscopy, mt-sDNA, FIT, and FOBT in the electronic medical record. Demographic and socioeconomic variables were collected. Inclusion criterion was age 50-75. Exclusion criteria were diagnostic testing, prior total colectomy, diagnosis of hereditary cancer syndrome, and inflammatory bowel disease.
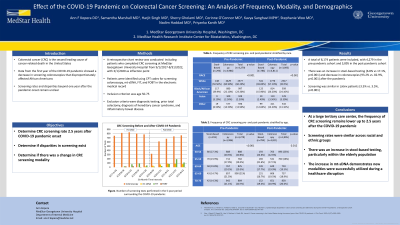
Results: A total of 8,174 patients were included, with 4,279 in the pre-pandemic cohort and 3,895 in the post-pandemic cohort. There was an increase in stool-based testing (6.8% vs 17.1%, p< 0.001) and decrease in colonoscopies (93.2% vs. 82.9%, p< 0.001) after the pandemic. Screening was stable in Latinx patients (3.5% vs. 3.5%, p< 0.001) and African American patients (23.3% vs. 24.1%, p=0.154). The proportion of African American patients screened with colonoscopy increased (22.1% vs. 26.2%), while stool-based testing decreased (39.9% vs. 15.9%). The percentage of older patients screened with stool-based testing increased for ages 65-69 (14.7% vs. 16.7%) and 70-75 (14.3% vs. 19.4%). In both pre- and post-pandemic groups, patients were more likely to be employed (55.8% vs. 61%, p< 0.001), married (63.1 vs. 60%, p< 0.001), have private insurance (67.6% vs. 70.4%, p< 0.05), have a primary care provider (96.9% vs. 91.6%, p< 0.001), and speak English (98.2% vs. 98.1%, p=0.534).
Discussion: At a large tertiary care center, the frequency of CRC screening remains lower up to 2.5 years after the COVID-19 pandemic. There was an increase in stool-based testing, particularly within the elderly population. The increase in mt-sDNA demonstrates new modalities were successfully utilized during a healthcare disruption.

Disclosures:
Ann Kopera, DO1, Samantha Marshall, MD1, Harjit Singh, MD1, Sherry Gholami, MD1, Corinne O'Connor, MD1, Kavya Sanghavi, MPH2, Stephanie M. Woo, MD1, Nadim Haddad, MD1, Priyanka Kanth, MD, MS1. P1752 - Effect of the COVID-19 Pandemic on Colorectal Cancer Screening: An Analysis of Frequency, Modality, and Demographics, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Washington, DC; 2MedStar Health Research Institute Center for Biostatistics, Washington, DC
Introduction: Colorectal cancer (CRC) is the second leading cause of cancer-related death in the United States. Data from the first year of the COVID-19 pandemic showed a decrease in screening colonoscopies that disproportionately affected African Americans. This study sought to determine the frequency, modality, and demographics of CRC screening two and a half years after the pandemic.
Methods: A retrospective chart review was conducted which included patients who completed colorectal cancer screening at MedStar Georgetown University Hospital from 9/1/2017-8/31/2022. March 1, 2020 was used as an inflection point. Patients were identified using CPT codes for screening colonoscopy, mt-sDNA, FIT, and FOBT in the electronic medical record. Demographic and socioeconomic variables were collected. Inclusion criterion was age 50-75. Exclusion criteria were diagnostic testing, prior total colectomy, diagnosis of hereditary cancer syndrome, and inflammatory bowel disease.
Results: A total of 8,174 patients were included, with 4,279 in the pre-pandemic cohort and 3,895 in the post-pandemic cohort. There was an increase in stool-based testing (6.8% vs 17.1%, p< 0.001) and decrease in colonoscopies (93.2% vs. 82.9%, p< 0.001) after the pandemic. Screening was stable in Latinx patients (3.5% vs. 3.5%, p< 0.001) and African American patients (23.3% vs. 24.1%, p=0.154). The proportion of African American patients screened with colonoscopy increased (22.1% vs. 26.2%), while stool-based testing decreased (39.9% vs. 15.9%). The percentage of older patients screened with stool-based testing increased for ages 65-69 (14.7% vs. 16.7%) and 70-75 (14.3% vs. 19.4%). In both pre- and post-pandemic groups, patients were more likely to be employed (55.8% vs. 61%, p< 0.001), married (63.1 vs. 60%, p< 0.001), have private insurance (67.6% vs. 70.4%, p< 0.05), have a primary care provider (96.9% vs. 91.6%, p< 0.001), and speak English (98.2% vs. 98.1%, p=0.534).
Discussion: At a large tertiary care center, the frequency of CRC screening remains lower up to 2.5 years after the COVID-19 pandemic. There was an increase in stool-based testing, particularly within the elderly population. The increase in mt-sDNA demonstrates new modalities were successfully utilized during a healthcare disruption.

Figure: Figure. Number of screening tests performed in the 5-year period surrounding the COVID-19 pandemic. The dashed line indicates the onset of the pandemic. The Y-axis indicates number of tests performed and the X-axis is six-month time intervals. Orange represents colonoscopy, yellow represents mt-sDNA, green represents FIT, and red represents FOBT.
Disclosures:
Ann Kopera indicated no relevant financial relationships.
Samantha Marshall indicated no relevant financial relationships.
Harjit Singh indicated no relevant financial relationships.
Sherry Gholami indicated no relevant financial relationships.
Corinne O'Connor indicated no relevant financial relationships.
Kavya Sanghavi indicated no relevant financial relationships.
Stephanie Woo indicated no relevant financial relationships.
Nadim Haddad indicated no relevant financial relationships.
Priyanka Kanth indicated no relevant financial relationships.
Ann Kopera, DO1, Samantha Marshall, MD1, Harjit Singh, MD1, Sherry Gholami, MD1, Corinne O'Connor, MD1, Kavya Sanghavi, MPH2, Stephanie M. Woo, MD1, Nadim Haddad, MD1, Priyanka Kanth, MD, MS1. P1752 - Effect of the COVID-19 Pandemic on Colorectal Cancer Screening: An Analysis of Frequency, Modality, and Demographics, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
