Monday Poster Session
Category: Colorectal Cancer Prevention
P1760 - The Economic Impact of a Blood-Based Glycoproteomic Test for Early Detection of Colorectal Cancer
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Alex Vanotti, MBA
InterVenn Biosciences
Arvada, CO
Presenting Author(s)
Alex Vanotti, MBA1, Andrea Mich, BA2, Dharini Chandrasekar, DO, MPH2, Alex Lindell, 2, Daniel Serie, MS2, Mike Fried, MBA, MHS3, Blake Long, MD, MBA4, Nik Sheng Ding, MBBS, PhD5, Daniel Hommes, MD, PhD2
1InterVenn Biosciences, Seattle, WA; 2InterVenn Biosciences, South San Francisco, CA; 3Alva10, Chapel Hill, NC; 4Alva10, Durham, NC; 5St. Vincent’s Hospital, East Melbourne, Victoria, Australia
Introduction: Despite existing innovative screening methods, colorectal cancer (CRC) still poses a significant risk for cancer-related deaths. Recently, a new blood-based test assessing the host immune response to developing CRC through glycoproteomic profiling has emerged. Our study aimed to assess the potential health and economic impact of this non-invasive approach to CRC detection in a commercial payer population.
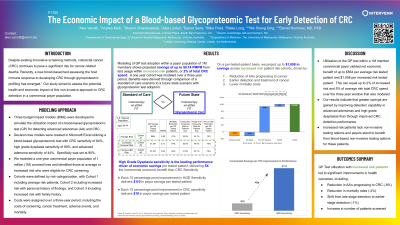
Methods: We developed three budget impact models (BIMs) to simulate the utilization impact of a blood-based glycoproteomic test for detecting advanced adenomas (AA) and CRC. We modeled a one-year commercial payer population of 1 million (1M) covered lives and identified those at average or increased risk who were eligible for CRC screening (Figure 1). Cohorts were defined by risk categorization, with Cohort 1 including average risk patients, Cohort 2 including increased risk with personal history of findings, and Cohort 3 including increased risk with family history. Costs were assigned to these patient cohorts over a three-year period, including the costs of screening, cancer treatment, adverse events, and mortality.
Results: The BIMs showed a net savings of $0.13 per member per month (PMPM) for the 1M patient population, including average and increased risk patients. On a per tested patient basis, adoption of the glycoproteomic test led to savings of $64, $501, and $547 for Cohorts 1, 2, and 3, respectively at a $500 test cost. Savings were driven primarily by a reduction in AAs that progressed to cancer (-11%), lower CRC treatment costs due to earlier stage disease detection (-3%), and reductions in mortality (-5%). Cancer incidence was reduced by 4%. Total colonoscopy procedures increased slightly (0.3%) due a net gain in the number of people screened, some of whom required a follow up colonoscopy. Across patient risk categorization, greater net payer savings were found among the increased risk cohorts ($0.06 PMPM) than the average risk cohort ($0.04).
Discussion: The addition of a novel glycoproteomic test to a CRC screening program could yield a net economic benefit for payers in addition to improved health outcomes. This economic benefit would be driven by a reduction in CRC treatment costs and a decrease in AA that progresses to cancer. By adopting this glycoproteomic testing approach, payers could improve patient outcomes while also reducing costs, making it a compelling strategy for enhancing CRC screening and prevention efforts.

Disclosures:
Alex Vanotti, MBA1, Andrea Mich, BA2, Dharini Chandrasekar, DO, MPH2, Alex Lindell, 2, Daniel Serie, MS2, Mike Fried, MBA, MHS3, Blake Long, MD, MBA4, Nik Sheng Ding, MBBS, PhD5, Daniel Hommes, MD, PhD2. P1760 - The Economic Impact of a Blood-Based Glycoproteomic Test for Early Detection of Colorectal Cancer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1InterVenn Biosciences, Seattle, WA; 2InterVenn Biosciences, South San Francisco, CA; 3Alva10, Chapel Hill, NC; 4Alva10, Durham, NC; 5St. Vincent’s Hospital, East Melbourne, Victoria, Australia
Introduction: Despite existing innovative screening methods, colorectal cancer (CRC) still poses a significant risk for cancer-related deaths. Recently, a new blood-based test assessing the host immune response to developing CRC through glycoproteomic profiling has emerged. Our study aimed to assess the potential health and economic impact of this non-invasive approach to CRC detection in a commercial payer population.
Methods: We developed three budget impact models (BIMs) to simulate the utilization impact of a blood-based glycoproteomic test for detecting advanced adenomas (AA) and CRC. We modeled a one-year commercial payer population of 1 million (1M) covered lives and identified those at average or increased risk who were eligible for CRC screening (Figure 1). Cohorts were defined by risk categorization, with Cohort 1 including average risk patients, Cohort 2 including increased risk with personal history of findings, and Cohort 3 including increased risk with family history. Costs were assigned to these patient cohorts over a three-year period, including the costs of screening, cancer treatment, adverse events, and mortality.
Results: The BIMs showed a net savings of $0.13 per member per month (PMPM) for the 1M patient population, including average and increased risk patients. On a per tested patient basis, adoption of the glycoproteomic test led to savings of $64, $501, and $547 for Cohorts 1, 2, and 3, respectively at a $500 test cost. Savings were driven primarily by a reduction in AAs that progressed to cancer (-11%), lower CRC treatment costs due to earlier stage disease detection (-3%), and reductions in mortality (-5%). Cancer incidence was reduced by 4%. Total colonoscopy procedures increased slightly (0.3%) due a net gain in the number of people screened, some of whom required a follow up colonoscopy. Across patient risk categorization, greater net payer savings were found among the increased risk cohorts ($0.06 PMPM) than the average risk cohort ($0.04).
Discussion: The addition of a novel glycoproteomic test to a CRC screening program could yield a net economic benefit for payers in addition to improved health outcomes. This economic benefit would be driven by a reduction in CRC treatment costs and a decrease in AA that progresses to cancer. By adopting this glycoproteomic testing approach, payers could improve patient outcomes while also reducing costs, making it a compelling strategy for enhancing CRC screening and prevention efforts.

Figure: Figure 1. Model methodology using patient risk cohorts.
Disclosures:
Alex Vanotti: InterVenn Biosciences – Employee.
Andrea Mich: InterVenn Biosciences – Employee.
Dharini Chandrasekar: InterVenn Biosciences – Employee.
Alex Lindell: InterVenn Biosciences – Employee.
Daniel Serie indicated no relevant financial relationships.
Mike Fried: Intervenn Biosciences – Consultant.
Blake Long: InterVenn – Consultant.
Nik Sheng Ding indicated no relevant financial relationships.
Daniel Hommes: InterVenn Biosciences – Employee.
Alex Vanotti, MBA1, Andrea Mich, BA2, Dharini Chandrasekar, DO, MPH2, Alex Lindell, 2, Daniel Serie, MS2, Mike Fried, MBA, MHS3, Blake Long, MD, MBA4, Nik Sheng Ding, MBBS, PhD5, Daniel Hommes, MD, PhD2. P1760 - The Economic Impact of a Blood-Based Glycoproteomic Test for Early Detection of Colorectal Cancer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
