Monday Poster Session
Category: Colorectal Cancer Prevention
P1766 - Assessing for Racial and Ethnic Disparities in Initial Average Risk Screening Colonoscopy Quality Metrics in a Large Military Gastroenterology Fellowship Program
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Carl Kay, MD
San Antonio Uniformed Services Health Education Consortium (SAUSHEC)
San Antonio, TX
Presenting Author(s)
Carl Kay, MD, Zachary Eagle, MD, John Gancayco, MD, Charles Miller, MD, Geoffrey Bader, MD
San Antonio Uniformed Services Health Education Consortium (SAUSHEC), San Antonio, TX
Introduction: Colorectal cancer (CRC) is the second overall leading cause of cancer mortality in the United States, though the burden of CRC varies across racial and ethnic groups. Colonoscopy is an effective procedure for CRC prevention but requires high quality performance. Given limited literature examining colonoscopy quality metrics across racial and ethnic groups, we sought to assess the impact of these demographics in our open-access, universal healthcare system.
Methods: We performed a retrospective review of initial average-risk screening colonoscopies performed between July 2019 and September 2022 at two military treatment facilities. Adenoma detection rate (ADR) was defined as the removal of ≥1 adenomatous polyp. Serrated polyp detection rate (SDR) was defined as the removal of ≥1 sessile serrated lesion, traditional serrated adenoma, or hyperplastic polyp ≥10mm in size. Advanced adenoma detection rate (AADR) was defined as the removal of ≥1 precancerous polyp ≥10mm in size, villous morphology, traditional serrated adenoma, and/or high-grade dysplasia. The adenomas per colonoscopy (APC) rate was calculated.
Results: A total of 2165 colonoscopies met inclusion criteria. Most patients were white (58.4%), followed by African American (AA; 20.1%) and Asian Pacific Islander (AAPI; 4.9%) (Table 1); 16.6% of patients identified as Hispanic (Table 1). Fellow involvement, adequate bowel preparation, cecal intubation rates, and mean withdrawal times were equivalent across racial and ethnic groups. ADR, SDR, and APC were lower in the AA group compared to the white group (p< 0.05; Table 1), but not the AADR. Hispanic patients had a lower SDR and AADR compared to non-Hispanic patients (p< 0.05; Table 1), but equivalent ADR and APC. In multivariate analysis, the ADR and SDR for AA were significantly lower compared to whites (adjusted OR for ADR 0.75; 95% CI 0.59-0.94, adjusted OR for SDR 0.46; 95% CI 0.31-0.69); the SDR for Hispanics was significantly lower compared to non-Hispanics (adjusted OR 0.54 for SDR; 95% CI 0.36-0.82).
Discussion: Each racial and ethnic group surpassed guideline colonoscopy quality standards; however, there were variable rates in adenoma detection. Prior literature has been mixed regarding the association between race and adenoma detection. Our universal healthcare system and high procedure quality metrics may provide insights into intrinsic differences in racial and ethnic precancerous polyp prevalence rates, but require prospective multicenter validation.

Disclosures:
Carl Kay, MD, Zachary Eagle, MD, John Gancayco, MD, Charles Miller, MD, Geoffrey Bader, MD. P1766 - Assessing for Racial and Ethnic Disparities in Initial Average Risk Screening Colonoscopy Quality Metrics in a Large Military Gastroenterology Fellowship Program, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
San Antonio Uniformed Services Health Education Consortium (SAUSHEC), San Antonio, TX
Introduction: Colorectal cancer (CRC) is the second overall leading cause of cancer mortality in the United States, though the burden of CRC varies across racial and ethnic groups. Colonoscopy is an effective procedure for CRC prevention but requires high quality performance. Given limited literature examining colonoscopy quality metrics across racial and ethnic groups, we sought to assess the impact of these demographics in our open-access, universal healthcare system.
Methods: We performed a retrospective review of initial average-risk screening colonoscopies performed between July 2019 and September 2022 at two military treatment facilities. Adenoma detection rate (ADR) was defined as the removal of ≥1 adenomatous polyp. Serrated polyp detection rate (SDR) was defined as the removal of ≥1 sessile serrated lesion, traditional serrated adenoma, or hyperplastic polyp ≥10mm in size. Advanced adenoma detection rate (AADR) was defined as the removal of ≥1 precancerous polyp ≥10mm in size, villous morphology, traditional serrated adenoma, and/or high-grade dysplasia. The adenomas per colonoscopy (APC) rate was calculated.
Results: A total of 2165 colonoscopies met inclusion criteria. Most patients were white (58.4%), followed by African American (AA; 20.1%) and Asian Pacific Islander (AAPI; 4.9%) (Table 1); 16.6% of patients identified as Hispanic (Table 1). Fellow involvement, adequate bowel preparation, cecal intubation rates, and mean withdrawal times were equivalent across racial and ethnic groups. ADR, SDR, and APC were lower in the AA group compared to the white group (p< 0.05; Table 1), but not the AADR. Hispanic patients had a lower SDR and AADR compared to non-Hispanic patients (p< 0.05; Table 1), but equivalent ADR and APC. In multivariate analysis, the ADR and SDR for AA were significantly lower compared to whites (adjusted OR for ADR 0.75; 95% CI 0.59-0.94, adjusted OR for SDR 0.46; 95% CI 0.31-0.69); the SDR for Hispanics was significantly lower compared to non-Hispanics (adjusted OR 0.54 for SDR; 95% CI 0.36-0.82).
Discussion: Each racial and ethnic group surpassed guideline colonoscopy quality standards; however, there were variable rates in adenoma detection. Prior literature has been mixed regarding the association between race and adenoma detection. Our universal healthcare system and high procedure quality metrics may provide insights into intrinsic differences in racial and ethnic precancerous polyp prevalence rates, but require prospective multicenter validation.

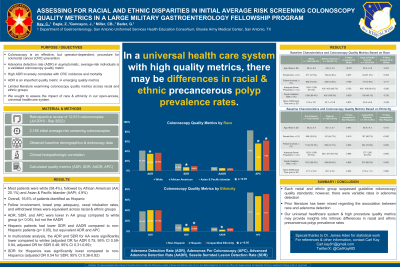
Figure: A: Colonoscopy quality metrics by race
B: Colonoscopy quality metrics by ethnicity
ADR, adenoma detection rate; SDR, serrated polyp detection rate; AADR, advanced adenoma detection rate; APC, adenomas per colonoscopy
B: Colonoscopy quality metrics by ethnicity
ADR, adenoma detection rate; SDR, serrated polyp detection rate; AADR, advanced adenoma detection rate; APC, adenomas per colonoscopy
Disclosures:
Carl Kay indicated no relevant financial relationships.
Zachary Eagle indicated no relevant financial relationships.
John Gancayco indicated no relevant financial relationships.
Charles Miller indicated no relevant financial relationships.
Geoffrey Bader indicated no relevant financial relationships.
Carl Kay, MD, Zachary Eagle, MD, John Gancayco, MD, Charles Miller, MD, Geoffrey Bader, MD. P1766 - Assessing for Racial and Ethnic Disparities in Initial Average Risk Screening Colonoscopy Quality Metrics in a Large Military Gastroenterology Fellowship Program, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
