Monday Poster Session
Category: Colorectal Cancer Prevention
P1774 - Risk of Colorectal Cancer in Incarcerated Patients With Inflammatory Bowel Disease in the United States: A Population-Based Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Temitope Olasehinde, MD
Case Western Reserve University / University Hospitals
Cleveland, OH
Presenting Author(s)
Temitope Olasehinde, MD1, Jaime A. Perez, PhD2, Vibhu Chittajallu, MD1, Jeffry Katz, MD3, Emad Mansoor, MD1, Gregory Cooper, MD3
1Case Western Reserve University / University Hospitals, Cleveland, OH; 2University Hospitals Clinical Research Center, Cleveland, OH; 3Case Western Reserve/UHCMC, Cleveland, OH
Introduction: Patients with inflammatory bowel disease (IBD) are at significantly increased risk of developing colorectal cancer (CRC). Despite the decline in incidence of IBD-associated CRC due to improvements in CRC surveillance programs and therapeutic advancements, prior studies show there remain significant disparities amongst vulnerable populations, such as incarcerated patients. This study is the first to assess the risk of CRC in incarcerated patients with IBD using a large population-based database.
Methods: We used a large federated de-identified health research network, TriNetX, with data sourced from 80 healthcare organizations (HCO) within the United States. We identified patients with a diagnosis of IBD based on International Classification of Diseases (ICD)10 codes between 2007-2023, and stratified based on a record of imprisonment. Available clinical data, including demographics, comorbid conditions, procedure history, medication use, and the outcome of CRC were collected. We compared prevalence and incidence of CRC after IBD diagnosis in incarcerated patients with IBD to a control cohort without a history of incarceration. Outcome risk was assessed using odds ratios and 95% confidence intervals.
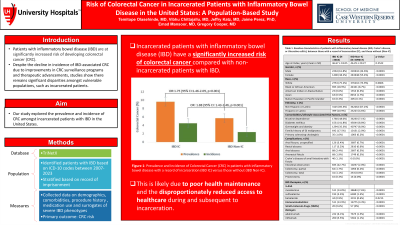
Results: We found a total of 512,680 patients with IBD. Among them, 3,660 IBD patients were incarcerated (IC) and the remaining 509,017 individuals were non-incarcerated (non-IC). 349 IBD patients in the IC group developed CRC after IBD diagnosis, whereas 13,535 developed CRC in the non-IC group. Compared to their non-IC counterparts, IC individuals with IBD were more likely to be male (61.8 % vs 44.6 %, p< 0.0001), non-Hispanic/Latino (85.3% vs 10.9%, p< 0.0001), and had higher prevalence of risk factors for CRC (p< 0.0001) (Table 1). Surrogates of severe IBD phenotypes such as peri-anal and fistulizing disease were also significantly higher in the IC group compared to the non-IC group (P< 0.001). For the primary outcome of CRC risk in patients with IBD, the IC group had a significantly higher prevalence (9.6% vs 5.7%, OR=1.75; 95% CI: 1.46-2.09, p< 0.001) and incidence (4.5% vs 2.4%, OR=1.88; 95% CI: 1.43-2.46, p< 0.001) compared to the non-IC group (Figure 1).
Discussion: To our knowledge, this is the first large retrospective cohort study to demonstrate increased CRC incidence in IBD patients who have been incarcerated. This is likely due to poor health maintenance in these individuals and the disproportionately reduced access to health care services during and subsequent to incarceration.

Disclosures:
Temitope Olasehinde, MD1, Jaime A. Perez, PhD2, Vibhu Chittajallu, MD1, Jeffry Katz, MD3, Emad Mansoor, MD1, Gregory Cooper, MD3. P1774 - Risk of Colorectal Cancer in Incarcerated Patients With Inflammatory Bowel Disease in the United States: A Population-Based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Case Western Reserve University / University Hospitals, Cleveland, OH; 2University Hospitals Clinical Research Center, Cleveland, OH; 3Case Western Reserve/UHCMC, Cleveland, OH
Introduction: Patients with inflammatory bowel disease (IBD) are at significantly increased risk of developing colorectal cancer (CRC). Despite the decline in incidence of IBD-associated CRC due to improvements in CRC surveillance programs and therapeutic advancements, prior studies show there remain significant disparities amongst vulnerable populations, such as incarcerated patients. This study is the first to assess the risk of CRC in incarcerated patients with IBD using a large population-based database.
Methods: We used a large federated de-identified health research network, TriNetX, with data sourced from 80 healthcare organizations (HCO) within the United States. We identified patients with a diagnosis of IBD based on International Classification of Diseases (ICD)10 codes between 2007-2023, and stratified based on a record of imprisonment. Available clinical data, including demographics, comorbid conditions, procedure history, medication use, and the outcome of CRC were collected. We compared prevalence and incidence of CRC after IBD diagnosis in incarcerated patients with IBD to a control cohort without a history of incarceration. Outcome risk was assessed using odds ratios and 95% confidence intervals.
Results: We found a total of 512,680 patients with IBD. Among them, 3,660 IBD patients were incarcerated (IC) and the remaining 509,017 individuals were non-incarcerated (non-IC). 349 IBD patients in the IC group developed CRC after IBD diagnosis, whereas 13,535 developed CRC in the non-IC group. Compared to their non-IC counterparts, IC individuals with IBD were more likely to be male (61.8 % vs 44.6 %, p< 0.0001), non-Hispanic/Latino (85.3% vs 10.9%, p< 0.0001), and had higher prevalence of risk factors for CRC (p< 0.0001) (Table 1). Surrogates of severe IBD phenotypes such as peri-anal and fistulizing disease were also significantly higher in the IC group compared to the non-IC group (P< 0.001). For the primary outcome of CRC risk in patients with IBD, the IC group had a significantly higher prevalence (9.6% vs 5.7%, OR=1.75; 95% CI: 1.46-2.09, p< 0.001) and incidence (4.5% vs 2.4%, OR=1.88; 95% CI: 1.43-2.46, p< 0.001) compared to the non-IC group (Figure 1).
Discussion: To our knowledge, this is the first large retrospective cohort study to demonstrate increased CRC incidence in IBD patients who have been incarcerated. This is likely due to poor health maintenance in these individuals and the disproportionately reduced access to health care services during and subsequent to incarceration.

Figure: Figure 1: Prevalence and Incidence of Colorectal Cancer (CRC) in patients with inflammatory bowel disease with a record of incarceration (IBD IC) versus those without (IBD Non-IC).
Disclosures:
Temitope Olasehinde indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Vibhu Chittajallu indicated no relevant financial relationships.
Jeffry Katz: Janssen, Pharmaceuticals – Grant/Research Support.
Emad Mansoor indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Temitope Olasehinde, MD1, Jaime A. Perez, PhD2, Vibhu Chittajallu, MD1, Jeffry Katz, MD3, Emad Mansoor, MD1, Gregory Cooper, MD3. P1774 - Risk of Colorectal Cancer in Incarcerated Patients With Inflammatory Bowel Disease in the United States: A Population-Based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
