Monday Poster Session
Category: Colorectal Cancer Prevention
P1779 - Statewide Burden of Colorectal Cancer and Its Attributable Risk Factors Across the United States Between 1990-2019: A Systematic and Comparative Benchmarking Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Hardik Dineshbhai Desai, MBBS
Gujarat Adani Institute of Medical Sciences
Bhuj, Gujarat, India
Presenting Author(s)
Award: Presidential Poster Award
Hardik Dineshbhai Desai, MBBS1, Mihir Prakash Shah, MD2, Bashar Attar, MD3, Victor O. Adedara, MS4, Rani Ratheesh, MBBS5, Tirath Patel, 6, Hardik YogeshKumar Patel, MBBS7, Ajay Kumar, MBBS8, Maham Kashif, MBBS9, Khawaja Muthammir Hassan, MBBS10, Muhammad Bilal Ibrahim, MD2
1Gujarat Adani Institute of Medical Sciences, Bhuj, Gujarat, India; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Cook County Health, Chicago, IL; 4St. George’s University School of Medicine, True Blue, Saint George, Grenada; 5Tamil Nadu Dr. M.G.R. Medical University, Chennai, Tamil Nadu, India; 6American University of Antigua, Osbourn, Saint John, Antigua and Barbuda; 7Sardar Multispecialty Hospital, Ahmedabad, Gujarat, India; 8Isra University, Hyderabad, Sindh, Pakistan; 9Khawaja Muhammad Safdar Medical College, Sialkot, Punjab, Pakistan; 10King Edward Medical University, Lahore, Punjab, Pakistan
Introduction: Colorectal Cancer (CRC) emerged as the second leading cause of cancer-related deaths in the United States, following lung cancer. Additionally, it ranked as the sixth leading cause of deaths overall, encompassing all causes in 2019. Previous studies have not produced comparable and consistent measures of total CRC burden at the state level.
Methods: The Global Burden of Disease (GBD) tool was used to compute CRC prevalence, incidence, and disability adjusted life years (DALYs), and its attributable risk factors stratified by age group, sex, and year from 1990-2019 for all U.S. residents using standardized data processing approaches and statistical modeling.
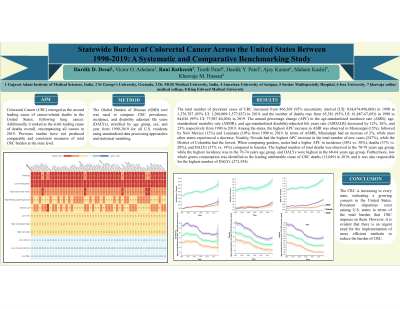
Results: The total number of prevalent cases of CRC increased from 866,569 (95% uncertainty interval [UI]: 834,474-896,068) in 1990 to 1,376,787 (95% UI: 1,200,009-1,577,837) in 2019, and the number of deaths rose from 65,581 (95% UI: 61,887-67,693) in 1990 to 84,026 (95% UI: 77,987-84,026) in 2019. The annual percentage change (APC) in the age-standardized incidence rate (ASIR), age-standardized mortality rate (ASMR), and age-standardized disability-adjusted life years rate (ASDALR) decreased by 12%, 26%, and 23% respectively from 1990 to 2019. Among the states, the highest APC increase in ASIR was observed in Mississippi (15%), followed by New Mexico (12%) and Louisiana (10%) from 1990 to 2019. In terms of ASMR, Mississippi had an increase of 2%, while most other states experienced a decrease. Notably, Nevada had the highest APC increase in the total number of new cases (247%), while the District of Columbia had the lowest. When comparing genders, males had a higher APC in incidence (58% vs. 38%), deaths (37% vs. 20%), and DALYs (37% vs. 19%) compared to females. The highest number of total deaths was observed in the 70-79 years age group, while the highest incidence was in the 70-74 years age group, and DALYs were highest in the 60-64 years age group. Furthermore, low whole grains consumption was identified as the leading attributable cause of CRC deaths (13,049) in 2019, and it was also responsible for the highest number of DALYs (273,554).
Discussion: The CRC is increasing in every state, indicating a growing concern in the United States. Persistent disparities exist among U.S. states in terms of the total burden that CRC imposes on them. However, it is evident that there is an urgent need for the implementation of more efficient methods to reduce the burden of CRC.

Disclosures:
Hardik Dineshbhai Desai, MBBS1, Mihir Prakash Shah, MD2, Bashar Attar, MD3, Victor O. Adedara, MS4, Rani Ratheesh, MBBS5, Tirath Patel, 6, Hardik YogeshKumar Patel, MBBS7, Ajay Kumar, MBBS8, Maham Kashif, MBBS9, Khawaja Muthammir Hassan, MBBS10, Muhammad Bilal Ibrahim, MD2. P1779 - Statewide Burden of Colorectal Cancer and Its Attributable Risk Factors Across the United States Between 1990-2019: A Systematic and Comparative Benchmarking Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Hardik Dineshbhai Desai, MBBS1, Mihir Prakash Shah, MD2, Bashar Attar, MD3, Victor O. Adedara, MS4, Rani Ratheesh, MBBS5, Tirath Patel, 6, Hardik YogeshKumar Patel, MBBS7, Ajay Kumar, MBBS8, Maham Kashif, MBBS9, Khawaja Muthammir Hassan, MBBS10, Muhammad Bilal Ibrahim, MD2
1Gujarat Adani Institute of Medical Sciences, Bhuj, Gujarat, India; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Cook County Health, Chicago, IL; 4St. George’s University School of Medicine, True Blue, Saint George, Grenada; 5Tamil Nadu Dr. M.G.R. Medical University, Chennai, Tamil Nadu, India; 6American University of Antigua, Osbourn, Saint John, Antigua and Barbuda; 7Sardar Multispecialty Hospital, Ahmedabad, Gujarat, India; 8Isra University, Hyderabad, Sindh, Pakistan; 9Khawaja Muhammad Safdar Medical College, Sialkot, Punjab, Pakistan; 10King Edward Medical University, Lahore, Punjab, Pakistan
Introduction: Colorectal Cancer (CRC) emerged as the second leading cause of cancer-related deaths in the United States, following lung cancer. Additionally, it ranked as the sixth leading cause of deaths overall, encompassing all causes in 2019. Previous studies have not produced comparable and consistent measures of total CRC burden at the state level.
Methods: The Global Burden of Disease (GBD) tool was used to compute CRC prevalence, incidence, and disability adjusted life years (DALYs), and its attributable risk factors stratified by age group, sex, and year from 1990-2019 for all U.S. residents using standardized data processing approaches and statistical modeling.
Results: The total number of prevalent cases of CRC increased from 866,569 (95% uncertainty interval [UI]: 834,474-896,068) in 1990 to 1,376,787 (95% UI: 1,200,009-1,577,837) in 2019, and the number of deaths rose from 65,581 (95% UI: 61,887-67,693) in 1990 to 84,026 (95% UI: 77,987-84,026) in 2019. The annual percentage change (APC) in the age-standardized incidence rate (ASIR), age-standardized mortality rate (ASMR), and age-standardized disability-adjusted life years rate (ASDALR) decreased by 12%, 26%, and 23% respectively from 1990 to 2019. Among the states, the highest APC increase in ASIR was observed in Mississippi (15%), followed by New Mexico (12%) and Louisiana (10%) from 1990 to 2019. In terms of ASMR, Mississippi had an increase of 2%, while most other states experienced a decrease. Notably, Nevada had the highest APC increase in the total number of new cases (247%), while the District of Columbia had the lowest. When comparing genders, males had a higher APC in incidence (58% vs. 38%), deaths (37% vs. 20%), and DALYs (37% vs. 19%) compared to females. The highest number of total deaths was observed in the 70-79 years age group, while the highest incidence was in the 70-74 years age group, and DALYs were highest in the 60-64 years age group. Furthermore, low whole grains consumption was identified as the leading attributable cause of CRC deaths (13,049) in 2019, and it was also responsible for the highest number of DALYs (273,554).
Discussion: The CRC is increasing in every state, indicating a growing concern in the United States. Persistent disparities exist among U.S. states in terms of the total burden that CRC imposes on them. However, it is evident that there is an urgent need for the implementation of more efficient methods to reduce the burden of CRC.

Figure: Burden of Colorectal Cancer across the United States. A: Trend of colorectal cancer between 1990-2019, B: Burden (age-standardized rate) of colorectal cancer in 2019, C: Heat map of Disability adjusted life years (DALYs) attributable risk factors for colorectal cancer.
Disclosures:
Hardik Dineshbhai Desai indicated no relevant financial relationships.
Mihir Prakash Shah indicated no relevant financial relationships.
Bashar Attar indicated no relevant financial relationships.
Victor O. Adedara indicated no relevant financial relationships.
Rani Ratheesh indicated no relevant financial relationships.
Tirath Patel indicated no relevant financial relationships.
Hardik YogeshKumar Patel indicated no relevant financial relationships.
Ajay Kumar indicated no relevant financial relationships.
Maham Kashif indicated no relevant financial relationships.
Khawaja Muthammir Hassan indicated no relevant financial relationships.
Muhammad Bilal Ibrahim indicated no relevant financial relationships.
Hardik Dineshbhai Desai, MBBS1, Mihir Prakash Shah, MD2, Bashar Attar, MD3, Victor O. Adedara, MS4, Rani Ratheesh, MBBS5, Tirath Patel, 6, Hardik YogeshKumar Patel, MBBS7, Ajay Kumar, MBBS8, Maham Kashif, MBBS9, Khawaja Muthammir Hassan, MBBS10, Muhammad Bilal Ibrahim, MD2. P1779 - Statewide Burden of Colorectal Cancer and Its Attributable Risk Factors Across the United States Between 1990-2019: A Systematic and Comparative Benchmarking Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

