Monday Poster Session
Category: Colorectal Cancer Prevention
P1788 - Trouble Grew: Clinical Challenges with Gastrointestinal Large Cell Neuroendocrine Carcinomas
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall

Tripti Nagar, MD
Wayne State University
Detroit, MI
Presenting Author(s)
Tripti Nagar, MD1, Alaa Taha, MD2, Vatsal Khanna, MD3, Trishya Reddy, MD4, Evangelos Bistas, MD4, Issam Turk, MD5
1Wayne State University, Detroit, MI; 2Wayne State University/Ascension Providence Rochester Hospital, Rochester, MI; 3Wayne State University School of Medicine, Rochester Hills, MI; 4Wayne State University, Rochester, MI; 5Ascension Providence Rochester Hospital, Rochester, MI
Introduction: LCNECs are uncommon colorectal malignancies with a poor prognosis due to aggressive disease spread at the time of diagnosis. Extraintestinal presentations are rare and colorectal carcinoma screening (CRCS) is usually directed at identifying adenocarcinoma. These tumors are clinically subtle, posing a diagnostic dilemma.
Case Description/Methods: We present three cases of unconventional presentations leading to a diagnosis of aggressive LCNEC.
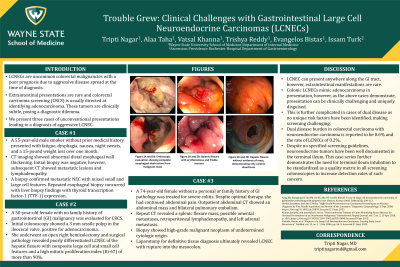
Case 1: A 55-year-old male smoker without prior medical history presented with fatigue, dysphagia, nausea, night sweats, and a 15-pound weight loss over one month. CT imaging showed abnormal distal esophageal wall thickening. Initial biopsy was negative, however, subsequent CT showed metastatic lesions and lymphadenopathy. A biopsy confirmed metastatic NEC with mixed small and large cell features. Repeated esophageal biopsy concurred with liver biopsy findings with thyroid transcription factor-1 (TTF-1) expression.
Case 2: A 50-year-old female with no family history of gastrointestinal (GI) malignancy was evaluated for CRCS. Study findings showed a 3 mm sessile polyp in the ileocecal valve, positive for adenocarcinoma. She underwent an open right hemicolectomy and surgical pathology revealed poorly differentiated LCNEC of the hepatic flexure with composite large cell and small cell features and a high mitotic proliferation index (Ki-67) of more than 90%.
Case 3: A 74-year-old female without a personal or family history of GI pathology was treated for severe colitis. Despite optimal therapy, she had continued abdominal pain. Outpatient abdominal CT showed an abdominal mass and bilateral pulmonary embolism. Repeat CT revealed a splenic flexure mass, possible omental metastases, retroperitoneal lymphadenopathy, and left adrenal metastasis. Biopsy showed high-grade malignant neoplasm of undetermined cytologic origin. Laparotomy for definitive tissue diagnosis ultimately revealed LCNEC with rupture into the mesocolon.
Discussion: LCNEC can present anywhere along the GI tract, however, extraintestinal manifestations are rare. Colonic LCNECs mimic adenocarcinoma in presentation, however, as the above cases demonstrate, presentation can be clinically challenging and uniquely disguised. This is further complicated in cases of dual disease as no unique risk factors have been identified, making screening challenging. There are no standardized guidelines for screening patients for LCNEC nor treatment guidelines, posing an opportunity for further research.
Disclosures:
Tripti Nagar, MD1, Alaa Taha, MD2, Vatsal Khanna, MD3, Trishya Reddy, MD4, Evangelos Bistas, MD4, Issam Turk, MD5. P1788 - Trouble Grew: Clinical Challenges with Gastrointestinal Large Cell Neuroendocrine Carcinomas, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wayne State University, Detroit, MI; 2Wayne State University/Ascension Providence Rochester Hospital, Rochester, MI; 3Wayne State University School of Medicine, Rochester Hills, MI; 4Wayne State University, Rochester, MI; 5Ascension Providence Rochester Hospital, Rochester, MI
Introduction: LCNECs are uncommon colorectal malignancies with a poor prognosis due to aggressive disease spread at the time of diagnosis. Extraintestinal presentations are rare and colorectal carcinoma screening (CRCS) is usually directed at identifying adenocarcinoma. These tumors are clinically subtle, posing a diagnostic dilemma.
Case Description/Methods: We present three cases of unconventional presentations leading to a diagnosis of aggressive LCNEC.
Case 1: A 55-year-old male smoker without prior medical history presented with fatigue, dysphagia, nausea, night sweats, and a 15-pound weight loss over one month. CT imaging showed abnormal distal esophageal wall thickening. Initial biopsy was negative, however, subsequent CT showed metastatic lesions and lymphadenopathy. A biopsy confirmed metastatic NEC with mixed small and large cell features. Repeated esophageal biopsy concurred with liver biopsy findings with thyroid transcription factor-1 (TTF-1) expression.
Case 2: A 50-year-old female with no family history of gastrointestinal (GI) malignancy was evaluated for CRCS. Study findings showed a 3 mm sessile polyp in the ileocecal valve, positive for adenocarcinoma. She underwent an open right hemicolectomy and surgical pathology revealed poorly differentiated LCNEC of the hepatic flexure with composite large cell and small cell features and a high mitotic proliferation index (Ki-67) of more than 90%.
Case 3: A 74-year-old female without a personal or family history of GI pathology was treated for severe colitis. Despite optimal therapy, she had continued abdominal pain. Outpatient abdominal CT showed an abdominal mass and bilateral pulmonary embolism. Repeat CT revealed a splenic flexure mass, possible omental metastases, retroperitoneal lymphadenopathy, and left adrenal metastasis. Biopsy showed high-grade malignant neoplasm of undetermined cytologic origin. Laparotomy for definitive tissue diagnosis ultimately revealed LCNEC with rupture into the mesocolon.
Discussion: LCNEC can present anywhere along the GI tract, however, extraintestinal manifestations are rare. Colonic LCNECs mimic adenocarcinoma in presentation, however, as the above cases demonstrate, presentation can be clinically challenging and uniquely disguised. This is further complicated in cases of dual disease as no unique risk factors have been identified, making screening challenging. There are no standardized guidelines for screening patients for LCNEC nor treatment guidelines, posing an opportunity for further research.
Disclosures:
Tripti Nagar indicated no relevant financial relationships.
Alaa Taha indicated no relevant financial relationships.
Vatsal Khanna indicated no relevant financial relationships.
Trishya Reddy indicated no relevant financial relationships.
Evangelos Bistas indicated no relevant financial relationships.
Issam Turk indicated no relevant financial relationships.
Tripti Nagar, MD1, Alaa Taha, MD2, Vatsal Khanna, MD3, Trishya Reddy, MD4, Evangelos Bistas, MD4, Issam Turk, MD5. P1788 - Trouble Grew: Clinical Challenges with Gastrointestinal Large Cell Neuroendocrine Carcinomas, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
