Monday Poster Session
Category: Endoscopy Video Forum
P1800 - Next-Generation Hemostasis: Practical Applications of the Endoscopic Doppler Probe in Non-Variceal Upper GI Bleeding
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- SD
Sue Dong, MD
New York University Langone Medical Center
Presenting Author(s)
Sue Dong, MD1, Kimberly Cheng, MD1, Melissa Latorre, MD2
1New York University Langone Medical Center, New York, NY; 2NYU Langone Health, New York, NY
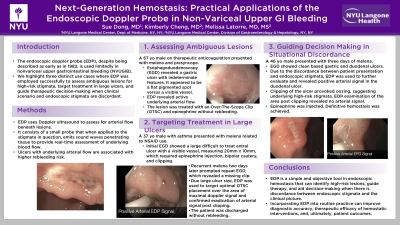
Introduction: The endoscopic doppler probe (EDP), despite being described as early as in 1982, is used limitedly in nonvariceal upper gastrointestinal bleeding (NVUGIB). This case report highlights three distinct cases where EDP was used successfully to assess ambiguous lesions for high-risk stigmata, target treatment in large ulcers, and guide therapeutic decision-making when clinical scenario and endoscopic stigmata are discordant.
Case Description/Methods: EDP uses Doppler ultrasound to assess for arterial flow beneath lesions. It consists of a small probe that when applied to the stigmata in question, emits sound waves penetrating tissue to provide real-time assessment of underlying blood flow. Ulcers with underlying arterial flow are associated with higher rebleeding risk.
Case 1:
A 67-year-old man presented with melena and presyncope. Esophagoduodenoscopy (EGD) revealed a gastric ulcer with indeterminate features. It appeared to be a flat pigmented spot versus a visible vessel. EDP revealed active underlying arterial flow. The lesion was treated with an Over-The-Scope Clip (OTSC) and epinephrine without rebleeding.
Case 2:
A 37-year-old man presented with melena related to NSAID use. Initial EGD showed a large difficult to treat antral ulcer with a visible vessel, measuring 20mm x 10mm, which required epinephrine injection, bipolar cautery, and clipping. Recurrent melena two days later prompted repeat EGD, which revealed a missing clip. Due large ulcer size, EDP was used to target optimal OTSC placement over the area of maximal doppler signal and confirmed eradication of arterial signal post clipping. The patient was discharged without rebleeding.
Case 3:
A 46-year-old man presented with three days of melena. EGD showed clean based gastric and duodenal ulcers. Due to the discordance between patient presentation and endoscopic stigmata, EDP was used to further evaluate and revealed positive arterial signal in the duodenal ulcer. Clipping of the ulcer provoked oozing, suggesting underlying high-risk stigmata. EDP examination of the area post clipping revealed no arterial signal. Epinephrine was injected. Definitive hemostasis was achieved.
Discussion: EDP is a simple and objective tool in endoscopic hemostasis that can identify high-risk lesions, guide therapy, and aid decision-making when there is discordance between endoscopic stigmata and the clinical picture. Incorporating EDP into routine practice can improve diagnostic accuracy, therapeutic efficacy of hemostatic interventions, and patient outcomes.
Disclosures:
Sue Dong, MD1, Kimberly Cheng, MD1, Melissa Latorre, MD2. P1800 - Next-Generation Hemostasis: Practical Applications of the Endoscopic Doppler Probe in Non-Variceal Upper GI Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1New York University Langone Medical Center, New York, NY; 2NYU Langone Health, New York, NY
Introduction: The endoscopic doppler probe (EDP), despite being described as early as in 1982, is used limitedly in nonvariceal upper gastrointestinal bleeding (NVUGIB). This case report highlights three distinct cases where EDP was used successfully to assess ambiguous lesions for high-risk stigmata, target treatment in large ulcers, and guide therapeutic decision-making when clinical scenario and endoscopic stigmata are discordant.
Case Description/Methods: EDP uses Doppler ultrasound to assess for arterial flow beneath lesions. It consists of a small probe that when applied to the stigmata in question, emits sound waves penetrating tissue to provide real-time assessment of underlying blood flow. Ulcers with underlying arterial flow are associated with higher rebleeding risk.
Case 1:
A 67-year-old man presented with melena and presyncope. Esophagoduodenoscopy (EGD) revealed a gastric ulcer with indeterminate features. It appeared to be a flat pigmented spot versus a visible vessel. EDP revealed active underlying arterial flow. The lesion was treated with an Over-The-Scope Clip (OTSC) and epinephrine without rebleeding.
Case 2:
A 37-year-old man presented with melena related to NSAID use. Initial EGD showed a large difficult to treat antral ulcer with a visible vessel, measuring 20mm x 10mm, which required epinephrine injection, bipolar cautery, and clipping. Recurrent melena two days later prompted repeat EGD, which revealed a missing clip. Due large ulcer size, EDP was used to target optimal OTSC placement over the area of maximal doppler signal and confirmed eradication of arterial signal post clipping. The patient was discharged without rebleeding.
Case 3:
A 46-year-old man presented with three days of melena. EGD showed clean based gastric and duodenal ulcers. Due to the discordance between patient presentation and endoscopic stigmata, EDP was used to further evaluate and revealed positive arterial signal in the duodenal ulcer. Clipping of the ulcer provoked oozing, suggesting underlying high-risk stigmata. EDP examination of the area post clipping revealed no arterial signal. Epinephrine was injected. Definitive hemostasis was achieved.
Discussion: EDP is a simple and objective tool in endoscopic hemostasis that can identify high-risk lesions, guide therapy, and aid decision-making when there is discordance between endoscopic stigmata and the clinical picture. Incorporating EDP into routine practice can improve diagnostic accuracy, therapeutic efficacy of hemostatic interventions, and patient outcomes.
Disclosures:
Sue Dong indicated no relevant financial relationships.
Kimberly Cheng indicated no relevant financial relationships.
Melissa Latorre: Medtronic – Consultant. Motus GI – Consultant. Olympus – Consultant. OVESCO – Consultant. VTI – Consultant.
Sue Dong, MD1, Kimberly Cheng, MD1, Melissa Latorre, MD2. P1800 - Next-Generation Hemostasis: Practical Applications of the Endoscopic Doppler Probe in Non-Variceal Upper GI Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
