Monday Poster Session
Category: Esophagus
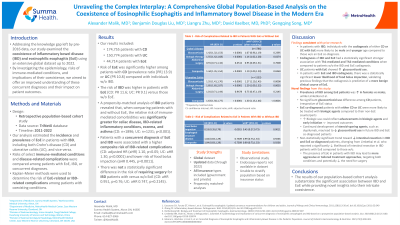
P1809 - Unraveling the Complex Interplay: A Comprehensive Global Population-Based Analysis on the Coexistence of Eosinophilic Esophagitis and Inflammatory Bowel Disease in the Modern Era
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Alexander K. Malik, MD
Summa Health System
Akron, OH
Presenting Author(s)
Alexander K. Malik, MD1, Benjamin D. Liu, MD2, Liangru Zhu, MD, PhD3, David Kaelber, MD, PhD, MPH4, Gengqing Song, MD5
1Summa Health System, Akron, OH; 2MetroHealth Medical Center, Cleveland, OH; 3Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China; 4Metro Health System, Cleveland, OH; 5MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Addressing the knowledge gap left by pre-2016 data, our study examined the coexistence of inflammatory bowel disease (IBD) and eosinophilic esophagitis (EOE) using an extensive global dataset up to 2022. By investigating the epidemiology, risks of immune-mediated conditions, and implications of their coexistence, we aimed to offer a comprehensive understanding of these concurrent diagnoses and their impact on patient outcomes.
Methods: A retrospective population-based cohort study was conducted using deidentified patient data from the TriNetX database (2011-2022). We estimated the incidence and prevalence of EOE in patients with IBD, including Crohn’s disease (CD) and ulcerative colitis (UC), and vice versa. Risks of select immune-mediated conditions were compared among patients with EOE, IBD, or concurrent diagnoses. Kaplan-Meier methods were used to determine the risk of EOE-related or IBD-related complications among patients with coexisting conditions.
Results: Our results included 174,755 patients with CD; 150,774 patients with UC; and 44,714 patients with EOE. The risk of EOE was significantly higher among patients with CD (prevalence ratio [PR] 13.7) or UC (PR 10.6) compared with individuals without IBD. The risk of IBD was higher in patients with EOE (CD: PR 11.6; UC: PR 9.1) versus those without either diagnosis. A propensity-matched analysis of IBD patients revealed that, when comparing patients with and without EOE, the relative risk of immune-mediated comorbidities was significantly greater for celiac disease, IBD-related inflammatory conditions, eczema, and asthma (CD: n=1896; UC: n=1231; p< 0.001). Patients with EOE and IBD were associated with a higher composite risk of IBD-related complications (CD: adjusted HR (aHR) 1.10, p< 0.05; UC: aHR 1.30, p< 0.0001) and lower risk of food bolus impaction (aHR 0.445, p=0.0011). There was no statistically significant difference in risk of requiring surgery for IBD patients with versus without EOE (CD: aHR 0.951, p=0.76; UC: aHR 0.747, p=0.2145).
Discussion: The results of our analysis substantiate the significant association between IBD and EOE while providing novel insights into their coexistence. These findings contribute to a deeper understanding of the complex interplay between EOE and IBD, and the implications of their concurrent diagnoses on patient complications. This pivotal discovery sets the stage for future research, refining patient care strategies, and driving innovation in the dynamic field of gastrointestinal research.
Disclosures:
Alexander K. Malik, MD1, Benjamin D. Liu, MD2, Liangru Zhu, MD, PhD3, David Kaelber, MD, PhD, MPH4, Gengqing Song, MD5. P1809 - Unraveling the Complex Interplay: A Comprehensive Global Population-Based Analysis on the Coexistence of Eosinophilic Esophagitis and Inflammatory Bowel Disease in the Modern Era, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Summa Health System, Akron, OH; 2MetroHealth Medical Center, Cleveland, OH; 3Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China; 4Metro Health System, Cleveland, OH; 5MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Addressing the knowledge gap left by pre-2016 data, our study examined the coexistence of inflammatory bowel disease (IBD) and eosinophilic esophagitis (EOE) using an extensive global dataset up to 2022. By investigating the epidemiology, risks of immune-mediated conditions, and implications of their coexistence, we aimed to offer a comprehensive understanding of these concurrent diagnoses and their impact on patient outcomes.
Methods: A retrospective population-based cohort study was conducted using deidentified patient data from the TriNetX database (2011-2022). We estimated the incidence and prevalence of EOE in patients with IBD, including Crohn’s disease (CD) and ulcerative colitis (UC), and vice versa. Risks of select immune-mediated conditions were compared among patients with EOE, IBD, or concurrent diagnoses. Kaplan-Meier methods were used to determine the risk of EOE-related or IBD-related complications among patients with coexisting conditions.
Results: Our results included 174,755 patients with CD; 150,774 patients with UC; and 44,714 patients with EOE. The risk of EOE was significantly higher among patients with CD (prevalence ratio [PR] 13.7) or UC (PR 10.6) compared with individuals without IBD. The risk of IBD was higher in patients with EOE (CD: PR 11.6; UC: PR 9.1) versus those without either diagnosis. A propensity-matched analysis of IBD patients revealed that, when comparing patients with and without EOE, the relative risk of immune-mediated comorbidities was significantly greater for celiac disease, IBD-related inflammatory conditions, eczema, and asthma (CD: n=1896; UC: n=1231; p< 0.001). Patients with EOE and IBD were associated with a higher composite risk of IBD-related complications (CD: adjusted HR (aHR) 1.10, p< 0.05; UC: aHR 1.30, p< 0.0001) and lower risk of food bolus impaction (aHR 0.445, p=0.0011). There was no statistically significant difference in risk of requiring surgery for IBD patients with versus without EOE (CD: aHR 0.951, p=0.76; UC: aHR 0.747, p=0.2145).
Discussion: The results of our analysis substantiate the significant association between IBD and EOE while providing novel insights into their coexistence. These findings contribute to a deeper understanding of the complex interplay between EOE and IBD, and the implications of their concurrent diagnoses on patient complications. This pivotal discovery sets the stage for future research, refining patient care strategies, and driving innovation in the dynamic field of gastrointestinal research.
Disclosures:
Alexander Malik indicated no relevant financial relationships.
Benjamin Liu indicated no relevant financial relationships.
Liangru Zhu indicated no relevant financial relationships.
David Kaelber: Becton, Dickinson and Company – Consultant. Dynavax Technologies Corporation – Consultant. Merck Sharp & Dohme Corporation – Consultant.
Gengqing Song indicated no relevant financial relationships.
Alexander K. Malik, MD1, Benjamin D. Liu, MD2, Liangru Zhu, MD, PhD3, David Kaelber, MD, PhD, MPH4, Gengqing Song, MD5. P1809 - Unraveling the Complex Interplay: A Comprehensive Global Population-Based Analysis on the Coexistence of Eosinophilic Esophagitis and Inflammatory Bowel Disease in the Modern Era, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
