Sunday Poster Session
Category: Biliary/Pancreas
P0053 - Trends and Outcomes in Timing of Cholecystectomy After ERCP in Patients with Choledocholithiasis in a Community Hospital
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Faizan Khalid, MD
Emory University School of Medicine
Atlanta, Georgia
Presenting Author(s)
Nida Khalid, MD1, Faizan Khalid, MD2, Sheza Malik, MD1, Mohammad Bilal, MD1, Atif Sohail, MD1, Ese Uwagbale, MD1, Ali Jaan, MD1, Ahmed Shehadah, MD1, Rutwik Sharma, MD3, Asim Mushtaq, MD1
1Rochester General Hospital, Rochester, NY; 2Emory University School of Medicine, Atlanta, GA; 3Unity Hospital, Rochester, NY
Introduction: The prevalence of common bile duct stones (CBDS) among individuals with symptomatic gallstones ranges from 10% to 20%, leading to complications such as cholangitis and pancreatitis. In the management of CBDS and gallbladder stones, cholecystectomy after ERCP is generally recommended. While early laparoscopic cholecystectomy is advised for severe biliary pancreatitis, the optimal timing for uncomplicated choledocholithiasis remains uncertain. Our objective was to examine the trends in management, assess complications, and determine re-hospitalization rates in patients who underwent ERCP for CBDS without concurrent cholecystectomy during index hospitalization in a community hospital.
Methods: A retrospective chart review was conducted on patients who underwent ERCP for CBDS at Rochester General Hospital NY from January 2017 to March 2023. Pts above 18 yrs of age with cholelithiasis were included.
Results: During the study period, a total of 161 ERCPs were performed for CBDS. The age range of the patients was 19 to 85 years, with females comprising 54% of the cohort.
Out of the 161 patients, 83 (52%) underwent cholecystectomy during the same admission. Among these patients, 16% were initially diagnosed with biliary pancreatitis. The median age and hospital stay for this group was 55 yrs and 5.3 days respectively. Temporal trends revealed a decrease in index cholecystectomy from 2020 to 2022, coinciding with the COVID-19 pandemic.
On the other hand, 78 (48%) patients did not undergo cholecystectomy during the index hospitalization. Among this group, 21% were initially diagnosed with biliary pancreatitis. The median age and hospital stay for patients without cholecystectomy during the index hospitalization was 60 yrs and 5.7 days respectively. Inpatient surgery consult was obtained for 67% of patients. Only 38 out of 78 pts eventually underwent outpatient cholecystectomy, with time intervals ranging from 1 week to 7 months. Among the 78 patients, 20 required readmission for recurrent CBDS or stent occlusion (11), pancreatitis (4), acute cholangitis/sepsis (3) or acute cholecystitis (2). 2 patients declined surgery, 3 were considered poor surgical candidates and 15 were lost to follow-up.
Discussion: Delays in cholecystectomy were linked to complications, rehospitalization, and loss to follow-up. Cholecystectomy during the index hospitalization did not significantly prolong the stay. Timely surgical consultation and cholecystectomy may reduce complications and be cost-effective.

Disclosures:
Nida Khalid, MD1, Faizan Khalid, MD2, Sheza Malik, MD1, Mohammad Bilal, MD1, Atif Sohail, MD1, Ese Uwagbale, MD1, Ali Jaan, MD1, Ahmed Shehadah, MD1, Rutwik Sharma, MD3, Asim Mushtaq, MD1. P0053 - Trends and Outcomes in Timing of Cholecystectomy After ERCP in Patients with Choledocholithiasis in a Community Hospital, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Emory University School of Medicine, Atlanta, GA; 3Unity Hospital, Rochester, NY
Introduction: The prevalence of common bile duct stones (CBDS) among individuals with symptomatic gallstones ranges from 10% to 20%, leading to complications such as cholangitis and pancreatitis. In the management of CBDS and gallbladder stones, cholecystectomy after ERCP is generally recommended. While early laparoscopic cholecystectomy is advised for severe biliary pancreatitis, the optimal timing for uncomplicated choledocholithiasis remains uncertain. Our objective was to examine the trends in management, assess complications, and determine re-hospitalization rates in patients who underwent ERCP for CBDS without concurrent cholecystectomy during index hospitalization in a community hospital.
Methods: A retrospective chart review was conducted on patients who underwent ERCP for CBDS at Rochester General Hospital NY from January 2017 to March 2023. Pts above 18 yrs of age with cholelithiasis were included.
Results: During the study period, a total of 161 ERCPs were performed for CBDS. The age range of the patients was 19 to 85 years, with females comprising 54% of the cohort.
Out of the 161 patients, 83 (52%) underwent cholecystectomy during the same admission. Among these patients, 16% were initially diagnosed with biliary pancreatitis. The median age and hospital stay for this group was 55 yrs and 5.3 days respectively. Temporal trends revealed a decrease in index cholecystectomy from 2020 to 2022, coinciding with the COVID-19 pandemic.
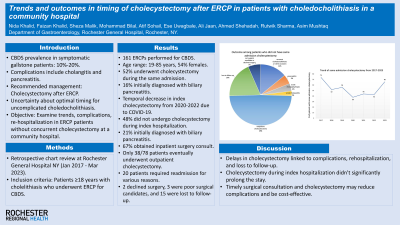
On the other hand, 78 (48%) patients did not undergo cholecystectomy during the index hospitalization. Among this group, 21% were initially diagnosed with biliary pancreatitis. The median age and hospital stay for patients without cholecystectomy during the index hospitalization was 60 yrs and 5.7 days respectively. Inpatient surgery consult was obtained for 67% of patients. Only 38 out of 78 pts eventually underwent outpatient cholecystectomy, with time intervals ranging from 1 week to 7 months. Among the 78 patients, 20 required readmission for recurrent CBDS or stent occlusion (11), pancreatitis (4), acute cholangitis/sepsis (3) or acute cholecystitis (2). 2 patients declined surgery, 3 were considered poor surgical candidates and 15 were lost to follow-up.
Discussion: Delays in cholecystectomy were linked to complications, rehospitalization, and loss to follow-up. Cholecystectomy during the index hospitalization did not significantly prolong the stay. Timely surgical consultation and cholecystectomy may reduce complications and be cost-effective.

Figure: Outcomes among patients who did not have same admission cholecystectomy after ERCP for choledocholithiasis
Disclosures:
Nida Khalid indicated no relevant financial relationships.
Faizan Khalid indicated no relevant financial relationships.
Sheza Malik indicated no relevant financial relationships.
Mohammad Bilal indicated no relevant financial relationships.
Atif Sohail indicated no relevant financial relationships.
Ese Uwagbale indicated no relevant financial relationships.
Ali Jaan indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Rutwik Sharma indicated no relevant financial relationships.
Asim Mushtaq indicated no relevant financial relationships.
Nida Khalid, MD1, Faizan Khalid, MD2, Sheza Malik, MD1, Mohammad Bilal, MD1, Atif Sohail, MD1, Ese Uwagbale, MD1, Ali Jaan, MD1, Ahmed Shehadah, MD1, Rutwik Sharma, MD3, Asim Mushtaq, MD1. P0053 - Trends and Outcomes in Timing of Cholecystectomy After ERCP in Patients with Choledocholithiasis in a Community Hospital, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
