Sunday Poster Session
Category: Biliary/Pancreas
P0076 - Bulky Burkitt Biliary Blockage: Lymphoma Resulting in Obstructive Jaundice
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Andrew Mertz, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Theodore Johnson, MD1, Ilan Vavilin, MD2, Andrew Mertz, MD1
1Walter Reed National Military Medical Center, Bethesda, MD; 2MedStar Georgetown University Hospital, Bethesda, MD
Introduction: Lymphoma as the etiology for obstructive jaundice accounts for 1-2% of all patients diagnosed with malignant biliary obstruction. A small fraction of these patients will present with obstructive jaundice as their only symptom, given this is an finding in advanced disease. Herein, we discuss a case of Burkitt lymphoma diagnosed in a renal transplant patient presenting with obstructive jaundice.
Case Description/Methods: A 61-year-old female with a past medical history of end stage renal disease secondary to longstanding hypertension who underwent deceased donor kidney transplant (DDKT) in 2008, on chronic immunosuppressive therapy with tacrolimus and mycophenolate presented to the emergency department with one week of nausea, pruritus, and painless jaundice. Her labs were notable for AST of 232 U/L, ALT of 258 U/L, total bilirubin of 2.9 mg/dL, and direct bilirubin of 2.3 mg/dL. Cross-sectional imaging revealed a large left perinephric mass with confluent periportal lymphadenopathy and marked intrahepatic biliary ductal dilation. Positron emission tomography revealed hypermetabolism within the perinephric mass and bulky adenopathy. Endoscopic retrograde cholangiopancreatography revealed a long segment of proximal common bile duct and hilar compression, to which stent was placed to relieve obstruction with subsequent normalization of her chemistries. Concurrently, she underwent IR-guided biopsy of the perinephric mass which demonstrated High-Grade B-Cell Lymphoma, with cytopathology confirming Burkitt’s Lymphoma. She was treated with systemic chemotherapy and her periportal adenopathy has resolved.
Discussion: Post-transplant lymphoproliferative disorders (PTLD) are lymphoid and/or plasmacytic proliferations that occur as a result of immunosuppression in the setting of solid organ or allogeneic hematopoietic cell transplantation. It is thought that latent reactivation of EBV-infected B-cells triggers this phenomenon, when the cytotoxic T-cell response is downregulated by immunosuppressant medications. Although lymphoma presenting as painless obstructive jaundice is uncommon, it should be included in the differential diagnosis, especially when risk factors such as immunosuppression and solid organ transplant are present. Additionally, relief of obstructive jaundice should be considered prior to starting chemotherapy if the severity of the obstruction is concerning for rapid progression and the development of cholangitis, which would delay the initiation of chemotherapy.

Disclosures:
Theodore Johnson, MD1, Ilan Vavilin, MD2, Andrew Mertz, MD1. P0076 - Bulky Burkitt Biliary Blockage: Lymphoma Resulting in Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Walter Reed National Military Medical Center, Bethesda, MD; 2MedStar Georgetown University Hospital, Bethesda, MD
Introduction: Lymphoma as the etiology for obstructive jaundice accounts for 1-2% of all patients diagnosed with malignant biliary obstruction. A small fraction of these patients will present with obstructive jaundice as their only symptom, given this is an finding in advanced disease. Herein, we discuss a case of Burkitt lymphoma diagnosed in a renal transplant patient presenting with obstructive jaundice.
Case Description/Methods: A 61-year-old female with a past medical history of end stage renal disease secondary to longstanding hypertension who underwent deceased donor kidney transplant (DDKT) in 2008, on chronic immunosuppressive therapy with tacrolimus and mycophenolate presented to the emergency department with one week of nausea, pruritus, and painless jaundice. Her labs were notable for AST of 232 U/L, ALT of 258 U/L, total bilirubin of 2.9 mg/dL, and direct bilirubin of 2.3 mg/dL. Cross-sectional imaging revealed a large left perinephric mass with confluent periportal lymphadenopathy and marked intrahepatic biliary ductal dilation. Positron emission tomography revealed hypermetabolism within the perinephric mass and bulky adenopathy. Endoscopic retrograde cholangiopancreatography revealed a long segment of proximal common bile duct and hilar compression, to which stent was placed to relieve obstruction with subsequent normalization of her chemistries. Concurrently, she underwent IR-guided biopsy of the perinephric mass which demonstrated High-Grade B-Cell Lymphoma, with cytopathology confirming Burkitt’s Lymphoma. She was treated with systemic chemotherapy and her periportal adenopathy has resolved.
Discussion: Post-transplant lymphoproliferative disorders (PTLD) are lymphoid and/or plasmacytic proliferations that occur as a result of immunosuppression in the setting of solid organ or allogeneic hematopoietic cell transplantation. It is thought that latent reactivation of EBV-infected B-cells triggers this phenomenon, when the cytotoxic T-cell response is downregulated by immunosuppressant medications. Although lymphoma presenting as painless obstructive jaundice is uncommon, it should be included in the differential diagnosis, especially when risk factors such as immunosuppression and solid organ transplant are present. Additionally, relief of obstructive jaundice should be considered prior to starting chemotherapy if the severity of the obstruction is concerning for rapid progression and the development of cholangitis, which would delay the initiation of chemotherapy.

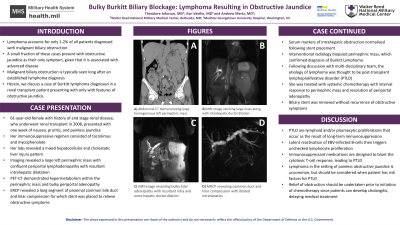
Figure: A) Abdominal CT demonstrating large homogeneous left perinephric mass
B) MRI image catching large mass along with intrahepatic ductal dilation
C) MRI image revealing bulky hilar adenopathy with resultant intra and extra-hepatic ductal dilation
D) MRCP reconstruction revealing common duct and hilar compression with dilated intrahepatics
B) MRI image catching large mass along with intrahepatic ductal dilation
C) MRI image revealing bulky hilar adenopathy with resultant intra and extra-hepatic ductal dilation
D) MRCP reconstruction revealing common duct and hilar compression with dilated intrahepatics
Disclosures:
Theodore Johnson indicated no relevant financial relationships.
Ilan Vavilin indicated no relevant financial relationships.
Andrew Mertz indicated no relevant financial relationships.
Theodore Johnson, MD1, Ilan Vavilin, MD2, Andrew Mertz, MD1. P0076 - Bulky Burkitt Biliary Blockage: Lymphoma Resulting in Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
