Sunday Poster Session
Category: Biliary/Pancreas
P0077 - A Rare Case of Solid Pseudopapillary Tumor of the Pancreas in a Male Patient
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Taher Jamali, MD
Henry Ford Health
Farmington Hills, MI
Presenting Author(s)
Taher Jamali, MD1, Georges Nassif, MD2, David Kwon, MD2, Robert Pompa, MD3
1Henry Ford Health, Farmington Hills, MI; 2Henry Ford Health, Detroit, MI; 3Henry Ford Hospital, Detroit, MI
Introduction: Solid pseudopapillary tumors (SPTs) of the pancreas only represent approximately 1% of all pancreatic neoplasms with less than 10% reported in male patients. Per literature review, male patients may have more aggressive disease and may require more radical resection1. Given the scarcity of reported cases, especially in males, it is important evaluate all cases for distinct features in presentation and surgical approach.
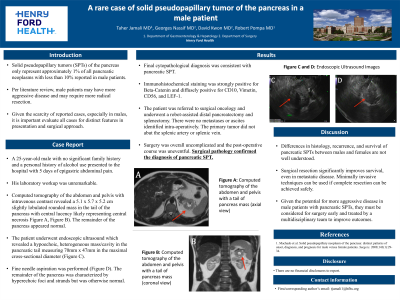
Case Description/Methods: A 25-year-old male with no significant family history and a personal history of alcohol use presented to the hospital with 5 days of epigastric abdominal pain. His laboratory workup was unremarkable. Computed tomography of the abdomen and pelvis with intravenous contrast revealed a 5.1 x 5.7 x 5.2 cm slightly lobulated rounded mass in the tail of the pancreas with central lucency likely representing central necrosis (1A, 1B). The remainder of the pancreas appeared normal. The patient underwent endoscopic ultrasound which revealed a hypoechoic, heterogeneous mass/cavity in the pancreatic tail measuring 70mm x 47mm in the maximal cross-sectional diameter (1C). Fine needle biopsy was performed (1D). The remainder of the pancreas was characterized by hyperechoic foci and strands but was otherwise normal. Final cytopathological diagnosis was consistent with pancreatic SPT. Immunohistochemical staining was strongly positive for Beta-Catenin and diffusely positive for CD10, Vimetin, CD56, and LEF-1. The patient was referred to surgical oncology and underwent a robot-assisted distal pancreatectomy and splenectomy. There were no metastases or ascites identified intra-operatively. The primary tumor did not abut the splenic artery or splenic vein. Surgery was overall uncomplicated and the post-operative course was uneventful. Surgical pathology confirmed the diagnosis of pancreatic SPT.
Discussion: Differences in histology, recurrence, and survival of pancreatic SPTs between males and females are not well understood. Surgical resection significantly improves survival, even in metastatic disease. Minimally invasive techniques can be used if complete resection can be achieved safely. Given the potential for more aggressive disease in male patients with pancreatic SPTs, they must be considered for surgery early and treated by a multidisciplinary team to improve outcomes.
1. Machado et al. Solid pseudopapillary neoplasm of the pancreas: distinct patterns of onset, diagnosis, and prognosis for male versus female patients. Surgery. 2008;143(1):29-34.

Disclosures:
Taher Jamali, MD1, Georges Nassif, MD2, David Kwon, MD2, Robert Pompa, MD3. P0077 - A Rare Case of Solid Pseudopapillary Tumor of the Pancreas in a Male Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Henry Ford Health, Farmington Hills, MI; 2Henry Ford Health, Detroit, MI; 3Henry Ford Hospital, Detroit, MI
Introduction: Solid pseudopapillary tumors (SPTs) of the pancreas only represent approximately 1% of all pancreatic neoplasms with less than 10% reported in male patients. Per literature review, male patients may have more aggressive disease and may require more radical resection1. Given the scarcity of reported cases, especially in males, it is important evaluate all cases for distinct features in presentation and surgical approach.
Case Description/Methods: A 25-year-old male with no significant family history and a personal history of alcohol use presented to the hospital with 5 days of epigastric abdominal pain. His laboratory workup was unremarkable. Computed tomography of the abdomen and pelvis with intravenous contrast revealed a 5.1 x 5.7 x 5.2 cm slightly lobulated rounded mass in the tail of the pancreas with central lucency likely representing central necrosis (1A, 1B). The remainder of the pancreas appeared normal. The patient underwent endoscopic ultrasound which revealed a hypoechoic, heterogeneous mass/cavity in the pancreatic tail measuring 70mm x 47mm in the maximal cross-sectional diameter (1C). Fine needle biopsy was performed (1D). The remainder of the pancreas was characterized by hyperechoic foci and strands but was otherwise normal. Final cytopathological diagnosis was consistent with pancreatic SPT. Immunohistochemical staining was strongly positive for Beta-Catenin and diffusely positive for CD10, Vimetin, CD56, and LEF-1. The patient was referred to surgical oncology and underwent a robot-assisted distal pancreatectomy and splenectomy. There were no metastases or ascites identified intra-operatively. The primary tumor did not abut the splenic artery or splenic vein. Surgery was overall uncomplicated and the post-operative course was uneventful. Surgical pathology confirmed the diagnosis of pancreatic SPT.
Discussion: Differences in histology, recurrence, and survival of pancreatic SPTs between males and females are not well understood. Surgical resection significantly improves survival, even in metastatic disease. Minimally invasive techniques can be used if complete resection can be achieved safely. Given the potential for more aggressive disease in male patients with pancreatic SPTs, they must be considered for surgery early and treated by a multidisciplinary team to improve outcomes.
1. Machado et al. Solid pseudopapillary neoplasm of the pancreas: distinct patterns of onset, diagnosis, and prognosis for male versus female patients. Surgery. 2008;143(1):29-34.

Figure: Figure 1: A) Axial computed tomography imaging of pancreatic solid pseduopapillary tumor (SPT); B) Coronal computed tomography imaging of pancreatic SPT; C) Endoscopic ultrasonographic view of pancreatic SPT; D) Endoscopic ultrasonographic view of fine needle biopsy of pancreatic SPT
Disclosures:
Taher Jamali indicated no relevant financial relationships.
Georges Nassif indicated no relevant financial relationships.
David Kwon indicated no relevant financial relationships.
Robert Pompa indicated no relevant financial relationships.
Taher Jamali, MD1, Georges Nassif, MD2, David Kwon, MD2, Robert Pompa, MD3. P0077 - A Rare Case of Solid Pseudopapillary Tumor of the Pancreas in a Male Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
