Sunday Poster Session
Category: Biliary/Pancreas
P0087 - Successful Management of Insulinoma by Computed Tomography Guided Ethanol Ablation
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Vinay Jahagirdar, MD
University of Missouri-Kansas City
Kansas City, MO
Presenting Author(s)
Vinay Jahagirdar, MD, Jagadish Koyi, MD, Noor Hassan, MD, Shourya Tadisina, MD, Thomas Bierman, MD, Rajib Bhattacharya, MD, Esmat Sadeddin, MD
University of Missouri-Kansas City, Kansas City, MO
Introduction: Insulinomas are rare pancreatic neuroendocrine tumors (NET), accounting for 1-2% of all pancreatic neoplasms. Most of them follow the ‘90%’ rule – 90% are benign, solitary and < 2 cm in size. We describe a case of insulinoma, diagnosed via biochemical tests, radiology and histopathology, and subsequently managed medically and by interventional radiology (IR).
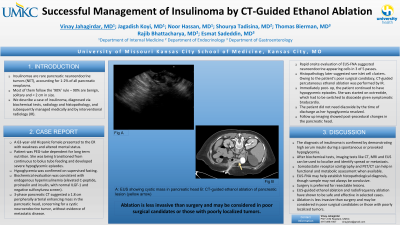
Case Description/Methods: A 63-year-old Hispanic female presented to the ER with weakness and altered mental status. The patient was PEG-tube dependent for long term nutrition. She was being transitioned from continuous to bolus tube feeding and developed severe hypoglycemic episodes. Hypoglycemia was confirmed on supervised fasting. Biochemical evaluation was consistent with endogenous hyperinsulinemia (elevated C-peptide, proinsulin and insulin, with normal ILGF-1 and negative sulfonylurea screen). 3-phase pancreatic CT suggested a 1.8 cm peripherally arterial enhancing mass in the pancreatic head, concerning for a cystic neuroendocrine tumor, without evidence of metastatic disease. Rapid onsite evaluation of EUS-FNA suggested neuroendocrine appearing cells in 3 of 5 passes. Histopathology later suggested rare islet cell clusters. Owing to the patient’s poor surgical candidacy, CT-guided percutaneous ethanol ablation was performed by IR. Immediately post-op, the patient continued to have hypogycemic episodes. She was started on octreotide, which had to be switched to diazoxide given symptomatic bradycardia. The patient did not need diazoxide by the time of discharge as her hypoglycemia resolved. Follow up imaging showed post-procedural changes in the pancreatic head.
Discussion: The diagnosis of insulinoma is confirmed by demonstrating high serum insulin during a spontaneous or provoked hypoglycemia. After biochemical tests, imaging tests like CT, MRI and EUS can be used to localize the suspected tumor and identify loco-regional spread or metastasis. Somatostatin receptor scintigraphy and PET/CT can help in functional and metabolic assessment when available. EUS-FNA may help establish histopathological diagnosis, though sample may not always be conclusive. Surgery is preferred for resectable lesions. EUS-guided ethanol ablation and radiofrequency ablation have shown to be safe and effective in selected cases, and are relatively newer approaches compared to CT-guided ablation. Ablation is less invasive than surgery and may be considered in poor surgical candidates or those with poorly localized tumors.

Disclosures:
Vinay Jahagirdar, MD, Jagadish Koyi, MD, Noor Hassan, MD, Shourya Tadisina, MD, Thomas Bierman, MD, Rajib Bhattacharya, MD, Esmat Sadeddin, MD. P0087 - Successful Management of Insulinoma by Computed Tomography Guided Ethanol Ablation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Missouri-Kansas City, Kansas City, MO
Introduction: Insulinomas are rare pancreatic neuroendocrine tumors (NET), accounting for 1-2% of all pancreatic neoplasms. Most of them follow the ‘90%’ rule – 90% are benign, solitary and < 2 cm in size. We describe a case of insulinoma, diagnosed via biochemical tests, radiology and histopathology, and subsequently managed medically and by interventional radiology (IR).
Case Description/Methods: A 63-year-old Hispanic female presented to the ER with weakness and altered mental status. The patient was PEG-tube dependent for long term nutrition. She was being transitioned from continuous to bolus tube feeding and developed severe hypoglycemic episodes. Hypoglycemia was confirmed on supervised fasting. Biochemical evaluation was consistent with endogenous hyperinsulinemia (elevated C-peptide, proinsulin and insulin, with normal ILGF-1 and negative sulfonylurea screen). 3-phase pancreatic CT suggested a 1.8 cm peripherally arterial enhancing mass in the pancreatic head, concerning for a cystic neuroendocrine tumor, without evidence of metastatic disease. Rapid onsite evaluation of EUS-FNA suggested neuroendocrine appearing cells in 3 of 5 passes. Histopathology later suggested rare islet cell clusters. Owing to the patient’s poor surgical candidacy, CT-guided percutaneous ethanol ablation was performed by IR. Immediately post-op, the patient continued to have hypogycemic episodes. She was started on octreotide, which had to be switched to diazoxide given symptomatic bradycardia. The patient did not need diazoxide by the time of discharge as her hypoglycemia resolved. Follow up imaging showed post-procedural changes in the pancreatic head.
Discussion: The diagnosis of insulinoma is confirmed by demonstrating high serum insulin during a spontaneous or provoked hypoglycemia. After biochemical tests, imaging tests like CT, MRI and EUS can be used to localize the suspected tumor and identify loco-regional spread or metastasis. Somatostatin receptor scintigraphy and PET/CT can help in functional and metabolic assessment when available. EUS-FNA may help establish histopathological diagnosis, though sample may not always be conclusive. Surgery is preferred for resectable lesions. EUS-guided ethanol ablation and radiofrequency ablation have shown to be safe and effective in selected cases, and are relatively newer approaches compared to CT-guided ablation. Ablation is less invasive than surgery and may be considered in poor surgical candidates or those with poorly localized tumors.

Figure: A: EUS showing cystic mass in pancreatic head B: CT-guided ethanol ablation of pancreatic lesion (yellow arrow)
Disclosures:
Vinay Jahagirdar indicated no relevant financial relationships.
Jagadish Koyi indicated no relevant financial relationships.
Noor Hassan indicated no relevant financial relationships.
Shourya Tadisina indicated no relevant financial relationships.
Thomas Bierman indicated no relevant financial relationships.
Rajib Bhattacharya indicated no relevant financial relationships.
Esmat Sadeddin indicated no relevant financial relationships.
Vinay Jahagirdar, MD, Jagadish Koyi, MD, Noor Hassan, MD, Shourya Tadisina, MD, Thomas Bierman, MD, Rajib Bhattacharya, MD, Esmat Sadeddin, MD. P0087 - Successful Management of Insulinoma by Computed Tomography Guided Ethanol Ablation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
