Sunday Poster Session
Category: Biliary/Pancreas
P0093 - A Rare Case of Autoimmune Pancreatitis in an HIV Patient
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Sylvia Keiser, DO
University of Texas Health Science Center at San Antonio
San Antonio, TX
Presenting Author(s)
Sylvia Keiser, DO1, Grace Hopp, DO, MBA2, Laura Rosenkranz, MD1
1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2UT Health San Antonio, San Antonio, TX
Introduction: Autoimmune pancreatitis (AIP) presents with diffuse pancreatic inflammation or as a focal mass and responds dramatically to glucocorticoid therapy. We present an unusual case of AIP in a patient with HIV.
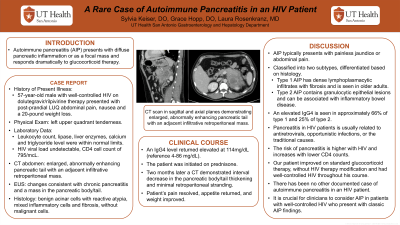
Case Description/Methods: A 57-year-old male with well-controlled HIV on dolutegravir/rilpivirine therapy presented with post-prandial, left upper quadrant abdominal pain. He had associated nausea and a 20-pound weight loss. Physical exam was remarkable for left upper quadrant tenderness. CT with contrast revealed an enlarged, abnormally enhancing pancreatic tail with an adjacent infiltrative retroperitoneal mass. He had a normal leukocyte count, lipase, liver enzymes, calcium and triglyceride level. His HIV viral load was undetectable and his CD4 cell count was 795/mcL.
An endoscopic ultrasound showed changes consistent with chronic pancreatitis and a mass in the pancreatic body/tail. Fine needle aspiration of the mass demonstrated benign acinar cells with reactive atypia, mixed inflammatory cells and fibrosis, without malignant cells. An IgG4 level was elevated at 114mg/dL (reference 4-86 mg/dL). The patient was initiated on prednisone. Two months later, CT demonstrated interval decrease in the pancreatic body/tail thickening and minimal retroperitoneal stranding. The patient’s pain resolved, appetite returned, and weight improved.
Discussion: Autoimmune pancreatitis typically presents with painless jaundice or abdominal pain. AIP is classified into two subtypes, differentiated based on histology. Type 1 AIP has dense lymphoplasmacytic infiltrates with fibrosis and is seen in older adults. Type 2 AIP contains granulocytic epithelial lesions and can be associated with inflammatory bowel disease. An elevated IgG4 is seen in approximately 66% of type 1 and 25% of type 2.
Pancreatitis in HIV patients is usually related to antiretrovirals, opportunistic infections, or the traditional causes. The risk of pancreatitis is higher with HIV and increases with lower CD4 counts. Our patient did improve on standard glucocorticoid therapy, without HIV therapy modification and had well-controlled HIV throughout his course. There has been no other documented case of autoimmune pancreatitis in an HIV patient. There have been other reports regarding pancreatic inflammation attributed to uncontrolled HIV that improves on antiretroviral therapy. It is crucial for clinicians to consider autoimmune pancreatitis in patients with well-controlled HIV who present with other classic AIP findings.

Disclosures:
Sylvia Keiser, DO1, Grace Hopp, DO, MBA2, Laura Rosenkranz, MD1. P0093 - A Rare Case of Autoimmune Pancreatitis in an HIV Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2UT Health San Antonio, San Antonio, TX
Introduction: Autoimmune pancreatitis (AIP) presents with diffuse pancreatic inflammation or as a focal mass and responds dramatically to glucocorticoid therapy. We present an unusual case of AIP in a patient with HIV.
Case Description/Methods: A 57-year-old male with well-controlled HIV on dolutegravir/rilpivirine therapy presented with post-prandial, left upper quadrant abdominal pain. He had associated nausea and a 20-pound weight loss. Physical exam was remarkable for left upper quadrant tenderness. CT with contrast revealed an enlarged, abnormally enhancing pancreatic tail with an adjacent infiltrative retroperitoneal mass. He had a normal leukocyte count, lipase, liver enzymes, calcium and triglyceride level. His HIV viral load was undetectable and his CD4 cell count was 795/mcL.
An endoscopic ultrasound showed changes consistent with chronic pancreatitis and a mass in the pancreatic body/tail. Fine needle aspiration of the mass demonstrated benign acinar cells with reactive atypia, mixed inflammatory cells and fibrosis, without malignant cells. An IgG4 level was elevated at 114mg/dL (reference 4-86 mg/dL). The patient was initiated on prednisone. Two months later, CT demonstrated interval decrease in the pancreatic body/tail thickening and minimal retroperitoneal stranding. The patient’s pain resolved, appetite returned, and weight improved.
Discussion: Autoimmune pancreatitis typically presents with painless jaundice or abdominal pain. AIP is classified into two subtypes, differentiated based on histology. Type 1 AIP has dense lymphoplasmacytic infiltrates with fibrosis and is seen in older adults. Type 2 AIP contains granulocytic epithelial lesions and can be associated with inflammatory bowel disease. An elevated IgG4 is seen in approximately 66% of type 1 and 25% of type 2.
Pancreatitis in HIV patients is usually related to antiretrovirals, opportunistic infections, or the traditional causes. The risk of pancreatitis is higher with HIV and increases with lower CD4 counts. Our patient did improve on standard glucocorticoid therapy, without HIV therapy modification and had well-controlled HIV throughout his course. There has been no other documented case of autoimmune pancreatitis in an HIV patient. There have been other reports regarding pancreatic inflammation attributed to uncontrolled HIV that improves on antiretroviral therapy. It is crucial for clinicians to consider autoimmune pancreatitis in patients with well-controlled HIV who present with other classic AIP findings.

Figure: CT scan in sagittal (A) and axial (B) planes demonstrating enlarged, abnormally enhancing pancreatic tail with an adjacent infiltrative retroperitoneal mass.
Disclosures:
Sylvia Keiser indicated no relevant financial relationships.
Grace Hopp indicated no relevant financial relationships.
Laura Rosenkranz indicated no relevant financial relationships.
Sylvia Keiser, DO1, Grace Hopp, DO, MBA2, Laura Rosenkranz, MD1. P0093 - A Rare Case of Autoimmune Pancreatitis in an HIV Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
