Sunday Poster Session
Category: Biliary/Pancreas
P0097 - Putting the US in Hemosuccus
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- JS
Jay Shah, DO
Saint Louis University
St. Louis, MO
Presenting Author(s)
Jay Shah, DO1, Ryan Plunkett, MD1, Eyad Gharaibeh, MD1, Hayden Rotramel, MD1, Jill E. Elwing, MD2
1Saint Louis University, St. Louis, MO; 2Washington University in St. Louis, St. Louis, MO
Introduction: Hemosuccus pancreaticus (HP) is a rare gastrointestinal (GI) condition classically defined as bleeding from the Ampulla of Vater. Although a rare cause of upper GI bleeding, it is associated with significant risk of mortality. While angiography remains the standard diagnostic and treatment strategy, we present a difficult case of HP requiring multiple imaging modalities to establish a diagnosis.
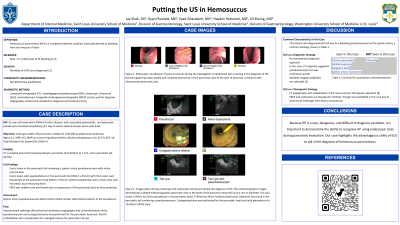
Case Description/Methods: A 41-year-old male with a history of Crohn disease and pancreatic pseudocyst presented complaining of abdominal pain. Labs exhibited no acute anemia, lipase of 254, and unremarkable hepatobiliary values. Computed tomography (CT) showed loculated pancreatic head pseudocyst, pancreatic duct dilation to 7 mm, and a pancreatic tail density. The pancreas was further evaluated by endoscopic ultrasound (EUS), revealing a 5.0 cm x 5.5 cm pancreatic head pseudocyst and a cystic lesion in the pancreatic tail containing a splenic artery pseudoaneurysm with active internal flow. ERCP was infeasible due to pseudocyst compression of the pancreatic duct. Interventional radiology (IR) used mesenteric angiography and coil embolization to treat the pseudoaneurysm. The patient recovered well and demonstrated improved pain control at a 3-month follow up.
Discussion: Our patient was diagnosed with HP in the setting of a pseudoaneurysm. HP is frequently associated with splenic artery pseudoaneurysm as the primary source of hemorrhage, as was seen in our patient. Our case was rather atypical as a pseudoaneurysm of this magnitude would commonly be associated with signs of GI bleeding, which our patient lacked. Identification of HP most commonly occurs via angiography, however in our case the initial suggestion of a lesion in the pancreatic tail originated in CT and the presence of HP was confirmed by EUS. ERCP does provide gastroenterologists an additional tool for treating this condition, although here endoscopic treatment was prohibited by compression of the pancreatic duct and relief was ultimately provided by standard angiographic embolization.
Because HP is a rare, dangerous, and difficult to diagnose condition, it is important to demonstrate the ability to recognize HP using endoscopic tools during pancreatic evaluation. Our case highlights this advantageous utility of EUS to aid in the diagnosis of hemosuccus pancreaticus.
References:
Yu P, Gong J. Hemosuccus pancreaticus: A mini-review. Ann Med Surg (Lond). 2018 Mar 9;28:45-48. doi: 10.1016/j.amsu.2018.03.002. PMID: 29744052; PMCID: PMC5938526.
Disclosures:
Jay Shah, DO1, Ryan Plunkett, MD1, Eyad Gharaibeh, MD1, Hayden Rotramel, MD1, Jill E. Elwing, MD2. P0097 - Putting the US in Hemosuccus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Louis University, St. Louis, MO; 2Washington University in St. Louis, St. Louis, MO
Introduction: Hemosuccus pancreaticus (HP) is a rare gastrointestinal (GI) condition classically defined as bleeding from the Ampulla of Vater. Although a rare cause of upper GI bleeding, it is associated with significant risk of mortality. While angiography remains the standard diagnostic and treatment strategy, we present a difficult case of HP requiring multiple imaging modalities to establish a diagnosis.
Case Description/Methods: A 41-year-old male with a history of Crohn disease and pancreatic pseudocyst presented complaining of abdominal pain. Labs exhibited no acute anemia, lipase of 254, and unremarkable hepatobiliary values. Computed tomography (CT) showed loculated pancreatic head pseudocyst, pancreatic duct dilation to 7 mm, and a pancreatic tail density. The pancreas was further evaluated by endoscopic ultrasound (EUS), revealing a 5.0 cm x 5.5 cm pancreatic head pseudocyst and a cystic lesion in the pancreatic tail containing a splenic artery pseudoaneurysm with active internal flow. ERCP was infeasible due to pseudocyst compression of the pancreatic duct. Interventional radiology (IR) used mesenteric angiography and coil embolization to treat the pseudoaneurysm. The patient recovered well and demonstrated improved pain control at a 3-month follow up.
Discussion: Our patient was diagnosed with HP in the setting of a pseudoaneurysm. HP is frequently associated with splenic artery pseudoaneurysm as the primary source of hemorrhage, as was seen in our patient. Our case was rather atypical as a pseudoaneurysm of this magnitude would commonly be associated with signs of GI bleeding, which our patient lacked. Identification of HP most commonly occurs via angiography, however in our case the initial suggestion of a lesion in the pancreatic tail originated in CT and the presence of HP was confirmed by EUS. ERCP does provide gastroenterologists an additional tool for treating this condition, although here endoscopic treatment was prohibited by compression of the pancreatic duct and relief was ultimately provided by standard angiographic embolization.
Because HP is a rare, dangerous, and difficult to diagnose condition, it is important to demonstrate the ability to recognize HP using endoscopic tools during pancreatic evaluation. Our case highlights this advantageous utility of EUS to aid in the diagnosis of hemosuccus pancreaticus.
References:
Yu P, Gong J. Hemosuccus pancreaticus: A mini-review. Ann Med Surg (Lond). 2018 Mar 9;28:45-48. doi: 10.1016/j.amsu.2018.03.002. PMID: 29744052; PMCID: PMC5938526.
Disclosures:
Jay Shah indicated no relevant financial relationships.
Ryan Plunkett indicated no relevant financial relationships.
Eyad Gharaibeh indicated no relevant financial relationships.
Hayden Rotramel indicated no relevant financial relationships.
Jill Elwing indicated no relevant financial relationships.
Jay Shah, DO1, Ryan Plunkett, MD1, Eyad Gharaibeh, MD1, Hayden Rotramel, MD1, Jill E. Elwing, MD2. P0097 - Putting the US in Hemosuccus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
