Sunday Poster Session
Category: Biliary/Pancreas
P0098 - Intraductal Papillary Mucinous Neoplasm Presenting With Gastropancreatic Fistula
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Ahmad Al-Dwairy, MBBS
MedStar Georgetown Washington Hospital Center
Washington, DC
Presenting Author(s)
Ahmad Al-Dwairy, MBBS1, Alexandra Piselli, MS2, Walid Chalhoub, MD3
1MedStar Georgetown Washington Hospital Center, Washington, DC; 2Georgetown University, Washington, DC; 3MedStar Georgetown University Hospital, Washington, DC
Introduction: Intraductal papillary mucinous neoplasms (IPMNs) are a rare group of cystic mucinous neoplasms that grow within the pancreatic ducts. They make up 1-2% of all exocrine pancreatic neoplasms and around 20-50% of all cystic pancreatic neoplasms. Fistulization is a complication of IPMN, which can occur due to malignant infiltration of nearby tissues, benign perforation, or inflammation. Herein, we present a rare case of IPMN presenting as a Gastropancreatic (GP) Fistula
Case Description/Methods: A 71-year-old female with a history of necrotizing pancreatitis resulting in major debridement in 2001 complicated by pancreatic insufficiency, diabetes mellites (DM), and chronic pancreatitis (CP) was followed by frequent endoscopic Ultrasound (EUS) to evaluate for known history of a pancreatic cyst. Due to demonstrated increasing size over time, multiple fine needle aspirations (FNA) were performed. Results were conflicting, ranging from findings of mucinous neoplasm to normal results negative for mucin
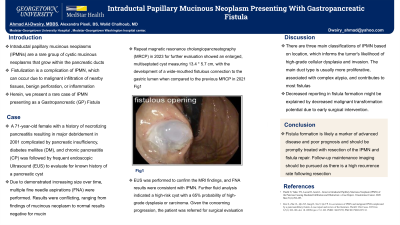
Repeat magnetic resonance cholangiopancreatography (MRCP) in 2023 for further evaluation showed an enlarged, multiseptated cyst measuring 13.4 * 5.7 cm, with the development of a wide-mouthed fistulous connection to the gastric lumen when compared to the previous MRCP in 2021 Fig1. EUS was performed to confirm the MRI findings, and FNA results were consistent with IPMN. Further fluid analysis indicated a high-risk cyst with a 65% probability of high-grade dysplasia or carcinoma.Given the concerning progression, the patient was referred for surgical evaluation
Discussion: There are three main classifications of IPMN based on location, which informs the tumor's likelihood of high-grade cellular dysplasia and invasion. The main duct type is usually more proliferative, associated with complex atypia, and contributes to most fistulas
Chronic pancreatitis, insulin-dependent diabetes, smoking, and family history have been identified as risk factors for IPMN and possibly fistula formation. Decreased reporting in fistula formation might be explained by decreased malignant transformation potential due to early surgical intervention.While the disease's natural course is unclear, longer life expectancy is thought to confer a greater risk of developing invasive cancer
Fistula formation is likely a marker of advanced disease and poor prognosis and should be promptly treated with resection of the IPMN and fistula repair. Follow-up maintenance imaging should be pursued as there is a high recurrence rate following resection

Disclosures:
Ahmad Al-Dwairy, MBBS1, Alexandra Piselli, MS2, Walid Chalhoub, MD3. P0098 - Intraductal Papillary Mucinous Neoplasm Presenting With Gastropancreatic Fistula, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1MedStar Georgetown Washington Hospital Center, Washington, DC; 2Georgetown University, Washington, DC; 3MedStar Georgetown University Hospital, Washington, DC
Introduction: Intraductal papillary mucinous neoplasms (IPMNs) are a rare group of cystic mucinous neoplasms that grow within the pancreatic ducts. They make up 1-2% of all exocrine pancreatic neoplasms and around 20-50% of all cystic pancreatic neoplasms. Fistulization is a complication of IPMN, which can occur due to malignant infiltration of nearby tissues, benign perforation, or inflammation. Herein, we present a rare case of IPMN presenting as a Gastropancreatic (GP) Fistula
Case Description/Methods: A 71-year-old female with a history of necrotizing pancreatitis resulting in major debridement in 2001 complicated by pancreatic insufficiency, diabetes mellites (DM), and chronic pancreatitis (CP) was followed by frequent endoscopic Ultrasound (EUS) to evaluate for known history of a pancreatic cyst. Due to demonstrated increasing size over time, multiple fine needle aspirations (FNA) were performed. Results were conflicting, ranging from findings of mucinous neoplasm to normal results negative for mucin
Repeat magnetic resonance cholangiopancreatography (MRCP) in 2023 for further evaluation showed an enlarged, multiseptated cyst measuring 13.4 * 5.7 cm, with the development of a wide-mouthed fistulous connection to the gastric lumen when compared to the previous MRCP in 2021 Fig1. EUS was performed to confirm the MRI findings, and FNA results were consistent with IPMN. Further fluid analysis indicated a high-risk cyst with a 65% probability of high-grade dysplasia or carcinoma.Given the concerning progression, the patient was referred for surgical evaluation
Discussion: There are three main classifications of IPMN based on location, which informs the tumor's likelihood of high-grade cellular dysplasia and invasion. The main duct type is usually more proliferative, associated with complex atypia, and contributes to most fistulas
Chronic pancreatitis, insulin-dependent diabetes, smoking, and family history have been identified as risk factors for IPMN and possibly fistula formation. Decreased reporting in fistula formation might be explained by decreased malignant transformation potential due to early surgical intervention.While the disease's natural course is unclear, longer life expectancy is thought to confer a greater risk of developing invasive cancer
Fistula formation is likely a marker of advanced disease and poor prognosis and should be promptly treated with resection of the IPMN and fistula repair. Follow-up maintenance imaging should be pursued as there is a high recurrence rate following resection

Figure: a wide-mouthed fistulous connection to the gastric lumen
Disclosures:
Ahmad Al-Dwairy indicated no relevant financial relationships.
Alexandra Piselli indicated no relevant financial relationships.
Walid Chalhoub indicated no relevant financial relationships.
Ahmad Al-Dwairy, MBBS1, Alexandra Piselli, MS2, Walid Chalhoub, MD3. P0098 - Intraductal Papillary Mucinous Neoplasm Presenting With Gastropancreatic Fistula, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
