Sunday Poster Session
Category: Biliary/Pancreas
P0104 - Pancreatitis Unveiled: A Case Report of IVIG-Induced Acute Pancreatitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Shiva F. Naidoo, MD
Geisinger Health System
Wilkes-Barre, PA
Presenting Author(s)
Shiva F. Naidoo, MD1, Lynzi Smith, BSc2, Parminder Dhingra, MD3, Hamzah Shariff, BA2, Sriram F. Chowdary, MD3, Divey Manocha, MD3
1Geisinger Health System, Wilkes-Barre, PA; 2Geisinger Commonwealth School of Medicine, Scranton, PA; 3Geisinger Health System, Scranton, PA
Introduction: Intravenous immunoglobulin (IVIG) therapy is a widely used treatment modality for various autoimmune and immunodeficiency disorders. Although generally considered safe, IVIG administration is not without potential adverse effects. Pancreatitis is a rare but recognized complication of IVIG therapy, with only a few documented cases reported in the literature. Here, we present a case of IVIG-induced pancreatitis in a patient with an autoimmune disorder, highlighting the importance of recognizing this uncommon but potentially serious adverse event.
Case Description/Methods:
A 70-year-old female with a history of Eosinophilic Asthma on Benralizumab and IVIG, type 2 diabetes, cholecystectomy, and hyperlipidemia presented with right upper quadrant abdominal pain radiating to her back and bloating for 1 day.
Hemodynamically was stable on room air except for a blood pressure 154/82 mmHg.
Medications were notable for Fexofenadine, Insulin, Fluticasone Propionate nasal spray, Levalbuterol, and Omeprazole.
Serology notable for leukocytosis, no anemia, normal renal and liver function, glucose of 150. Further labs were notable for serum lipase of 557, triglycerides of 222 HDL of 46, and normal IgG subclasses 1 to 4.
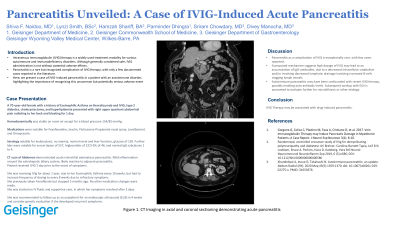
CT scan of Abdomen demonstrated acute interstitial edematous pancreatitis. Mild inflammation around the extrahepatic biliary system, likely reactive to adjacent pancreatitis.
Patient received IVIG 1 day prior to the onset of symptoms. She was receiving IVIg for about 1 year, due to her Eosinophilic Asthma every 10 weeks, but had to increase frequency of dosing to every 8 weeks due to refractory symptoms.
She previously taken Fenofibrate but stopped 5 months ago. No other medication changes were made.
She was started on IV fluids and supportive care, in which her symptoms resolved after 2 days.
She was recommended to follow up as an outpatient for an endoscopic ultrasound (EUS) in 4 weeks and consider genetic evaluation if she developed recurrent symptoms.
Discussion: Pancreatitis as a complication of IVIG is exceptionally rare, with few cases reported.
A proposed mechanism suggests high dosage of IVIG may lead to an accumulation of IgG-antibodies, due to a decreased intracellular catabolism and/or involving decreased lymphatic drainage involving increased B-cells clogging lymph vessels.
Autoimmune pancreatitis may have been confounded with recent IVIG therapy, possibly masking auto-antibody levels. Subsequent workup with EUS is warranted to evaluate further for microlithiasis or other etiology.

Disclosures:
Shiva F. Naidoo, MD1, Lynzi Smith, BSc2, Parminder Dhingra, MD3, Hamzah Shariff, BA2, Sriram F. Chowdary, MD3, Divey Manocha, MD3. P0104 - Pancreatitis Unveiled: A Case Report of IVIG-Induced Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Geisinger Health System, Wilkes-Barre, PA; 2Geisinger Commonwealth School of Medicine, Scranton, PA; 3Geisinger Health System, Scranton, PA
Introduction: Intravenous immunoglobulin (IVIG) therapy is a widely used treatment modality for various autoimmune and immunodeficiency disorders. Although generally considered safe, IVIG administration is not without potential adverse effects. Pancreatitis is a rare but recognized complication of IVIG therapy, with only a few documented cases reported in the literature. Here, we present a case of IVIG-induced pancreatitis in a patient with an autoimmune disorder, highlighting the importance of recognizing this uncommon but potentially serious adverse event.
Case Description/Methods:
A 70-year-old female with a history of Eosinophilic Asthma on Benralizumab and IVIG, type 2 diabetes, cholecystectomy, and hyperlipidemia presented with right upper quadrant abdominal pain radiating to her back and bloating for 1 day.
Hemodynamically was stable on room air except for a blood pressure 154/82 mmHg.
Medications were notable for Fexofenadine, Insulin, Fluticasone Propionate nasal spray, Levalbuterol, and Omeprazole.
Serology notable for leukocytosis, no anemia, normal renal and liver function, glucose of 150. Further labs were notable for serum lipase of 557, triglycerides of 222 HDL of 46, and normal IgG subclasses 1 to 4.
CT scan of Abdomen demonstrated acute interstitial edematous pancreatitis. Mild inflammation around the extrahepatic biliary system, likely reactive to adjacent pancreatitis.
Patient received IVIG 1 day prior to the onset of symptoms. She was receiving IVIg for about 1 year, due to her Eosinophilic Asthma every 10 weeks, but had to increase frequency of dosing to every 8 weeks due to refractory symptoms.
She previously taken Fenofibrate but stopped 5 months ago. No other medication changes were made.
She was started on IV fluids and supportive care, in which her symptoms resolved after 2 days.
She was recommended to follow up as an outpatient for an endoscopic ultrasound (EUS) in 4 weeks and consider genetic evaluation if she developed recurrent symptoms.
Discussion: Pancreatitis as a complication of IVIG is exceptionally rare, with few cases reported.
A proposed mechanism suggests high dosage of IVIG may lead to an accumulation of IgG-antibodies, due to a decreased intracellular catabolism and/or involving decreased lymphatic drainage involving increased B-cells clogging lymph vessels.
Autoimmune pancreatitis may have been confounded with recent IVIG therapy, possibly masking auto-antibody levels. Subsequent workup with EUS is warranted to evaluate further for microlithiasis or other etiology.

Figure: Acute intersitial pancreatitis observed on CT abdomen coronal and axial views
Disclosures:
Shiva Naidoo indicated no relevant financial relationships.
Lynzi Smith indicated no relevant financial relationships.
Parminder Dhingra indicated no relevant financial relationships.
Hamzah Shariff indicated no relevant financial relationships.
Sriram Chowdary indicated no relevant financial relationships.
Divey Manocha indicated no relevant financial relationships.
Shiva F. Naidoo, MD1, Lynzi Smith, BSc2, Parminder Dhingra, MD3, Hamzah Shariff, BA2, Sriram F. Chowdary, MD3, Divey Manocha, MD3. P0104 - Pancreatitis Unveiled: A Case Report of IVIG-Induced Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
