Sunday Poster Session
Category: Biliary/Pancreas
P0114 - Biliary Ductal Dilation from Altered Anatomy and Type IV Hiatal Hernia
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Samuel Purkey, DO
Allegheny Health Network
Pittsburgh, PA
Presenting Author(s)
Award: Presidential Poster Award
Samuel Purkey, DO, Oluwakemi Adewuyi, MD, Rachel Toney, MD
Allegheny Health Network, Pittsburgh, PA
Introduction: Biliary ductal dilation is a frequent consultation for gastroenterologist. Common etiologies include choledocholithiasis, biliary strictures, mass effect, and malignancy. We present an atypical case of a type IV hiatal hernia causing anatomical distortion leading to obstructive jaundice and biliary ductal dilation.
Case Description/Methods: We present an 80-year-old female presenting as a transfer with concerns for obstructive jaundice, biliary ductal dilation, and 2 days of abdominal pain. Initial labs revealed a normal CBC and BMP but an AST of 55 U/L, ALT of 98 U/L, ALP of 208 U/L, and total bilirubin of 3.3 mg/dL. A CT chest and abdomen with contrast revealed a large diaphragmatic hernia with small and large bowel, pancreas, and stomach content within the chest and biliary ductal dilation to 13 mm concerning for an obstructive process. An MRCP was obtained revealing severe biliary ductal dilation to 15 mm but no obvious stricture or stone.
Upon transfer, her labs improved to a bilirubin .8 mg/dL, but given her presentation and imaging, the plan was for an ERCP. However, a GIF scope was required for guide wire placement to assist with passage of the duodenoscope through the altered anatomy to identify the ampulla. After bile duct cannulation, dye injection revealed a "sigmoid" shaped common bile duct with proximal bile duct dilation, severe mid duct angulation, and normal distal common bile duct. There was no stricture, stone, or sludge present on occlusion cholangiogram or balloon sweeping. Due to the angulation, there was retained contrast in the proximal common bile duct, thus a 10 French by 9 cm plastic stent with single external and internal flap was placed to assist with drainage.
Following her ERCP, her symptoms resolved and her bilirubin remained normal. She was continued on pantoprazole therapy for her GERD secondary the hernia. Cardiothoracic surgery was consulted and recommended outpatient follow-up to discuss surgical management as definitive treatment of her type IV hiatal hernia.
Discussion: Biliary ductal dilation from severe hiatal hernias is uncommon, with only a few reported cases causing anatomical distortion leading to biliary ductal dilation and even pancreatitis. We present a case of a type IV hiatal hernia causing anatomical distortion and biliary obstruction. Work-up should include baseline labs, imaging, and consideration for endoscopic intervention in setting of ductal dilation and obstructive jaundice. Surgery remains the mainstay therapy for type IV hiatal hernias.

Disclosures:
Samuel Purkey, DO, Oluwakemi Adewuyi, MD, Rachel Toney, MD. P0114 - Biliary Ductal Dilation from Altered Anatomy and Type IV Hiatal Hernia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Samuel Purkey, DO, Oluwakemi Adewuyi, MD, Rachel Toney, MD
Allegheny Health Network, Pittsburgh, PA
Introduction: Biliary ductal dilation is a frequent consultation for gastroenterologist. Common etiologies include choledocholithiasis, biliary strictures, mass effect, and malignancy. We present an atypical case of a type IV hiatal hernia causing anatomical distortion leading to obstructive jaundice and biliary ductal dilation.
Case Description/Methods: We present an 80-year-old female presenting as a transfer with concerns for obstructive jaundice, biliary ductal dilation, and 2 days of abdominal pain. Initial labs revealed a normal CBC and BMP but an AST of 55 U/L, ALT of 98 U/L, ALP of 208 U/L, and total bilirubin of 3.3 mg/dL. A CT chest and abdomen with contrast revealed a large diaphragmatic hernia with small and large bowel, pancreas, and stomach content within the chest and biliary ductal dilation to 13 mm concerning for an obstructive process. An MRCP was obtained revealing severe biliary ductal dilation to 15 mm but no obvious stricture or stone.
Upon transfer, her labs improved to a bilirubin .8 mg/dL, but given her presentation and imaging, the plan was for an ERCP. However, a GIF scope was required for guide wire placement to assist with passage of the duodenoscope through the altered anatomy to identify the ampulla. After bile duct cannulation, dye injection revealed a "sigmoid" shaped common bile duct with proximal bile duct dilation, severe mid duct angulation, and normal distal common bile duct. There was no stricture, stone, or sludge present on occlusion cholangiogram or balloon sweeping. Due to the angulation, there was retained contrast in the proximal common bile duct, thus a 10 French by 9 cm plastic stent with single external and internal flap was placed to assist with drainage.
Following her ERCP, her symptoms resolved and her bilirubin remained normal. She was continued on pantoprazole therapy for her GERD secondary the hernia. Cardiothoracic surgery was consulted and recommended outpatient follow-up to discuss surgical management as definitive treatment of her type IV hiatal hernia.
Discussion: Biliary ductal dilation from severe hiatal hernias is uncommon, with only a few reported cases causing anatomical distortion leading to biliary ductal dilation and even pancreatitis. We present a case of a type IV hiatal hernia causing anatomical distortion and biliary obstruction. Work-up should include baseline labs, imaging, and consideration for endoscopic intervention in setting of ductal dilation and obstructive jaundice. Surgery remains the mainstay therapy for type IV hiatal hernias.

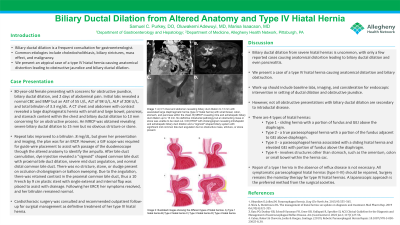
Figure: A: CT chest and abdomen revealing biliary duct dilation to 13 mm with associated large diaphragmatic hernia (type IV hiatal hernia) with small bowel, colon, stomach, and pancreas within the chest.
B: MRCP revealing intra and extrahepatic biliary duct dilation up to 15 mm. No definitive intraductal pathology but an obstructing mass or stone was unable to be ruled out.
C/D: ERCP with cholangiogram revealing intrahepatic and extrahepatic biliary duct dilation and a "sigmoid" shaped biliary system with significant mid common bile duct angulation but no obstructive mass, stricture, or stone present.
B: MRCP revealing intra and extrahepatic biliary duct dilation up to 15 mm. No definitive intraductal pathology but an obstructing mass or stone was unable to be ruled out.
C/D: ERCP with cholangiogram revealing intrahepatic and extrahepatic biliary duct dilation and a "sigmoid" shaped biliary system with significant mid common bile duct angulation but no obstructive mass, stricture, or stone present.
Disclosures:
Samuel Purkey indicated no relevant financial relationships.
Oluwakemi Adewuyi indicated no relevant financial relationships.
Rachel Toney indicated no relevant financial relationships.
Samuel Purkey, DO, Oluwakemi Adewuyi, MD, Rachel Toney, MD. P0114 - Biliary Ductal Dilation from Altered Anatomy and Type IV Hiatal Hernia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

