Sunday Poster Session
Category: Biliary/Pancreas
P0118 - Get Smashed! Not Your Typical Cause of Pancreatitis – The Mesenteritis Enigma
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
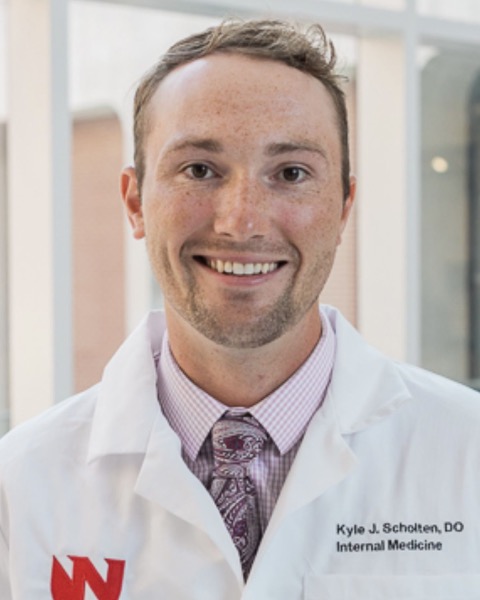
Kyle Scholten, DO
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Kyle Scholten, DO1, Kevin Brittan, MD1, Josh Warner, MD1, Patrick Twohig, MD, MPH1, Sarah Malik, MD2, Kathryn Hutchins, MD3
1University of Nebraska Medical Center, Omaha, NE; 2Nebraska Medical Center, Omaha, NE; 3UNMC / Nebraska Medicine, Omaha, NE
Introduction: Sclerosing mesenteritis (SM) is a rare, poorly understood inflammatory and fibrotic condition of the mesentery. Autoimmune diseases such as autoimmune pancreatitis and retroperitoneal fibrosis have been linked to SM. The diagnosis is made by laparoscopic biopsy but is often difficult to make given its non-specific symptom presentation (weight loss, abdominal pain) and ambiguous imaging findings, which may be confused for malignancy. Although associated with autoimmune pancreatitis, SM is not classically identified as a cause of pancreatitis. We present a case of recurrent acute pancreatitis secondary to sclerosing mesenteritis.
Case Description/Methods: A 52-year-old female with a history of cholecystectomy and biopsy-proven sclerosing mesenteritis presented to the hospital with epigastric pain - this was her fifth hospitalization with the same presentation in the prior four months. On admission, lipase was 532, with magnetic resonance cholangiopancreatography (MRCP) showing interstitial pancreatitis and irregularity of the main pancreatic duct with no focal biliary strictures or biliary duct dilation. Imaging also showed a soft tissue mass encasing the superior mesenteric artery, occluding the superior mesenteric vein and portal vein with associated cavernous transformation (Figure 1) – consistent with sclerosing mesenteritis. Social history was negative for alcohol and tobacco use. IgG4 levels were normal. Triglycerides were 479. Other work-up, including autoimmune testing and calcium levels, were normal/negative. She was not taking any pancreatitis-associated medications. Due to the mass effect of her SM on mesenteric vasculature, it was determined that ischemia was precipitant to her pancreatitis episodes. She was treated with prednisone acutely and transitioned to azathioprine as an outpatient without any subsequent episodes of pancreatitis and stability of the mass seen on CT approximately one-year post-hospitalization.
Discussion: Our case highlights a rare cause of abdominal pain and recurrent acute pancreatitis. Although difficult to diagnose, clinicians should include SM on the differential for atypical intra-abdominal mass and acute/recurrent pancreatitis. Mainstay of therapy includes prednisone and azathioprine or tamoxifen for three months, pending response. If symptoms persist, patients can undergo a trial of azathioprine or cyclophosphamide - if azathioprine fails to improve symptomatology.

Disclosures:
Kyle Scholten, DO1, Kevin Brittan, MD1, Josh Warner, MD1, Patrick Twohig, MD, MPH1, Sarah Malik, MD2, Kathryn Hutchins, MD3. P0118 - Get Smashed! Not Your Typical Cause of Pancreatitis – The Mesenteritis Enigma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Nebraska Medical Center, Omaha, NE; 2Nebraska Medical Center, Omaha, NE; 3UNMC / Nebraska Medicine, Omaha, NE
Introduction: Sclerosing mesenteritis (SM) is a rare, poorly understood inflammatory and fibrotic condition of the mesentery. Autoimmune diseases such as autoimmune pancreatitis and retroperitoneal fibrosis have been linked to SM. The diagnosis is made by laparoscopic biopsy but is often difficult to make given its non-specific symptom presentation (weight loss, abdominal pain) and ambiguous imaging findings, which may be confused for malignancy. Although associated with autoimmune pancreatitis, SM is not classically identified as a cause of pancreatitis. We present a case of recurrent acute pancreatitis secondary to sclerosing mesenteritis.
Case Description/Methods: A 52-year-old female with a history of cholecystectomy and biopsy-proven sclerosing mesenteritis presented to the hospital with epigastric pain - this was her fifth hospitalization with the same presentation in the prior four months. On admission, lipase was 532, with magnetic resonance cholangiopancreatography (MRCP) showing interstitial pancreatitis and irregularity of the main pancreatic duct with no focal biliary strictures or biliary duct dilation. Imaging also showed a soft tissue mass encasing the superior mesenteric artery, occluding the superior mesenteric vein and portal vein with associated cavernous transformation (Figure 1) – consistent with sclerosing mesenteritis. Social history was negative for alcohol and tobacco use. IgG4 levels were normal. Triglycerides were 479. Other work-up, including autoimmune testing and calcium levels, were normal/negative. She was not taking any pancreatitis-associated medications. Due to the mass effect of her SM on mesenteric vasculature, it was determined that ischemia was precipitant to her pancreatitis episodes. She was treated with prednisone acutely and transitioned to azathioprine as an outpatient without any subsequent episodes of pancreatitis and stability of the mass seen on CT approximately one-year post-hospitalization.
Discussion: Our case highlights a rare cause of abdominal pain and recurrent acute pancreatitis. Although difficult to diagnose, clinicians should include SM on the differential for atypical intra-abdominal mass and acute/recurrent pancreatitis. Mainstay of therapy includes prednisone and azathioprine or tamoxifen for three months, pending response. If symptoms persist, patients can undergo a trial of azathioprine or cyclophosphamide - if azathioprine fails to improve symptomatology.

Figure: Figure 1: Coronal computed tomography (CT) with contrast showing encasement of the superior mesenteric artery (red) by sclerosing mesenteritis mass (purple).
Disclosures:
Kyle Scholten indicated no relevant financial relationships.
Kevin Brittan indicated no relevant financial relationships.
Josh Warner indicated no relevant financial relationships.
Patrick Twohig: Bausch Health – Grant/Research Support.
Sarah Malik indicated no relevant financial relationships.
Kathryn Hutchins indicated no relevant financial relationships.
Kyle Scholten, DO1, Kevin Brittan, MD1, Josh Warner, MD1, Patrick Twohig, MD, MPH1, Sarah Malik, MD2, Kathryn Hutchins, MD3. P0118 - Get Smashed! Not Your Typical Cause of Pancreatitis – The Mesenteritis Enigma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

