Sunday Poster Session
Category: Biliary/Pancreas
P0124 - Autoimmune Pancreatitis Type 1 Presenting as a Pancreatic Mass in an Elderly Woman
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Jerapas Thongpiya, MD
Texas Tech University Health Sciences Center
Lubbock, TX
Presenting Author(s)
Jerapas Thongpiya, MD, Pitchaporn Yingchoncharoen, MD, Gandhi Lanke, MD, Meenu Sharma, MD, Kanak Das, MD
Texas Tech University Health Sciences Center, Lubbock, TX
Introduction: Autoimmune pancreatitis (AIP) is an uncommon cause of recurrent acute pancreatitis or painless jaundice. AIP is classified into type 1 as lymphoplasmacytic sclerosing pancreatitis from IgG-4 infiltration and type 2 as idiopathic duct centric pancreatitis. Type 1 AIP is the pancreatic manifestation of IgG-4 related disease. Comprehensive evaluation of the patient including clinical, imaging, serologic and histopathology is necessary for accurate diagnosis. Here, we report an unusual presentation of AIP type 1 presenting as a pancreas head mass.
Case Description/Methods: A 66-year-old woman with past medical history of hypothyroidism, hyperlipidemia, hypertension presented to the hospital with severe epigastric pain for the past 2-3 months, associated with 7-pound weight loss and jaundice. Physical examination was unremarkable except for icterus and epigastric tenderness. Labs were remarkable for elevated total bilirubin 9.5mg/dL, AST153 IU/L, ALT 144IU/L, ALP187IU/L, and elevated CA19-9 81.4 units/mL (< = 35 normal). CT abdomen showed slightly enlarged edematous distal body and tail of pancreas with minimal peripancreatic fat streaking. She underwent EUS which showed pancreas head mass with pancreatitis and CBD dilatation of 1cm. EUS-guided FNB of the mass was performed. ERCP showed a 4-cm biliary stricture in the lower third of the CBD with malignant appearance causing proximal CBD dilatation. ERCP brushing was done for cytology from the lower third of the CBD and a covered metal stent was placed. Pathology of pancreas head mass showed pancreatic parenchyma with dense lymphoplasmacytic infiltrate, storiform/pinwheel fibrosis, and focal obliterative phlebitis with greater than 10 IgG4+ plasma cells/HPF, while distal CBD brushing showed only reactive process. The findings were most consistent with AIP type 1; IgG4-related pancreatitis (IgG4-RP). She was started on prednisone 0.6 mg/kg/day for 1 month with slow taper. Her symptoms completely resolved along with normal liver enzymes in 1 month, and repeat MRI in 6 months showed resolution of pancreatic head mass and biliary dilatation.
Discussion: In our case, AIP type 1 presented as pancreas head mass mimicking malignancy. With the advent of EUS, FNB was possible to confirm the diagnosis of AIP. Accurate diagnosis of AIP is important to prevent unnecessary surgical resections. Corticosteroid is the mainstay treatment for AIP. Multidisciplinary team approach involving radiologist, advanced endoscopist, and pathologist is key in management of AIP.

Disclosures:
Jerapas Thongpiya, MD, Pitchaporn Yingchoncharoen, MD, Gandhi Lanke, MD, Meenu Sharma, MD, Kanak Das, MD. P0124 - Autoimmune Pancreatitis Type 1 Presenting as a Pancreatic Mass in an Elderly Woman, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Texas Tech University Health Sciences Center, Lubbock, TX
Introduction: Autoimmune pancreatitis (AIP) is an uncommon cause of recurrent acute pancreatitis or painless jaundice. AIP is classified into type 1 as lymphoplasmacytic sclerosing pancreatitis from IgG-4 infiltration and type 2 as idiopathic duct centric pancreatitis. Type 1 AIP is the pancreatic manifestation of IgG-4 related disease. Comprehensive evaluation of the patient including clinical, imaging, serologic and histopathology is necessary for accurate diagnosis. Here, we report an unusual presentation of AIP type 1 presenting as a pancreas head mass.
Case Description/Methods: A 66-year-old woman with past medical history of hypothyroidism, hyperlipidemia, hypertension presented to the hospital with severe epigastric pain for the past 2-3 months, associated with 7-pound weight loss and jaundice. Physical examination was unremarkable except for icterus and epigastric tenderness. Labs were remarkable for elevated total bilirubin 9.5mg/dL, AST153 IU/L, ALT 144IU/L, ALP187IU/L, and elevated CA19-9 81.4 units/mL (< = 35 normal). CT abdomen showed slightly enlarged edematous distal body and tail of pancreas with minimal peripancreatic fat streaking. She underwent EUS which showed pancreas head mass with pancreatitis and CBD dilatation of 1cm. EUS-guided FNB of the mass was performed. ERCP showed a 4-cm biliary stricture in the lower third of the CBD with malignant appearance causing proximal CBD dilatation. ERCP brushing was done for cytology from the lower third of the CBD and a covered metal stent was placed. Pathology of pancreas head mass showed pancreatic parenchyma with dense lymphoplasmacytic infiltrate, storiform/pinwheel fibrosis, and focal obliterative phlebitis with greater than 10 IgG4+ plasma cells/HPF, while distal CBD brushing showed only reactive process. The findings were most consistent with AIP type 1; IgG4-related pancreatitis (IgG4-RP). She was started on prednisone 0.6 mg/kg/day for 1 month with slow taper. Her symptoms completely resolved along with normal liver enzymes in 1 month, and repeat MRI in 6 months showed resolution of pancreatic head mass and biliary dilatation.
Discussion: In our case, AIP type 1 presented as pancreas head mass mimicking malignancy. With the advent of EUS, FNB was possible to confirm the diagnosis of AIP. Accurate diagnosis of AIP is important to prevent unnecessary surgical resections. Corticosteroid is the mainstay treatment for AIP. Multidisciplinary team approach involving radiologist, advanced endoscopist, and pathologist is key in management of AIP.

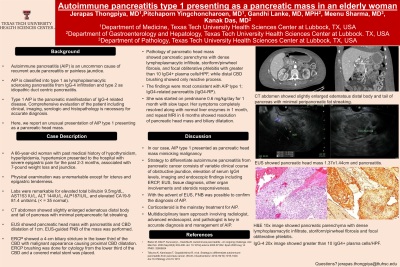
Figure: CT abdomen showed slightly enlarged edematous distal body and tail of pancreas with minimal peripancreatic fat streaking.
EUS showed pancreatic head mass 1.37x1.44cm and pancreatitis.
H&E 10x image showed pancreatic parenchyma with dense lymphoplasmacytic infiltrate, storiform/pinwheel fibrosis and focal obliterative phlebitis.
IgG-4 20x image showed greater than 10 IgG4+ plasma cells/HPF.
EUS showed pancreatic head mass 1.37x1.44cm and pancreatitis.
H&E 10x image showed pancreatic parenchyma with dense lymphoplasmacytic infiltrate, storiform/pinwheel fibrosis and focal obliterative phlebitis.
IgG-4 20x image showed greater than 10 IgG4+ plasma cells/HPF.
Disclosures:
Jerapas Thongpiya indicated no relevant financial relationships.
Pitchaporn Yingchoncharoen indicated no relevant financial relationships.
Gandhi Lanke indicated no relevant financial relationships.
Meenu Sharma indicated no relevant financial relationships.
Kanak Das indicated no relevant financial relationships.
Jerapas Thongpiya, MD, Pitchaporn Yingchoncharoen, MD, Gandhi Lanke, MD, Meenu Sharma, MD, Kanak Das, MD. P0124 - Autoimmune Pancreatitis Type 1 Presenting as a Pancreatic Mass in an Elderly Woman, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
