Sunday Poster Session
Category: Biliary/Pancreas
P0127 - Diagnostic Dilemma of Gallbladder Cancer vs Rare Cholecystitis/Cholangitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Michael Su, MD
HCA West Florida
Riverview, FL
Presenting Author(s)
Michael Su, MD1, Allyson Pagan, MD2, Viraj Modi, BS, DO2, Ruchir Paladiya, MBBS3, Bhavtosh Dedania, MD4
1HCA West Florida, Brandon, FL; 2HCA West Florida Brandon, Brandon, FL; 3UConn Health, Hartford, CT; 4HCA Florida Brandon Hospital, Brandon, FL
Introduction: Xanthogranulomatous Cholecystitis (XGC) is a rare type of cholecystitis that poses a diagnostic challenge. Cholangitis is an even rarer complication as only 5 such cases of XGC with cholangitis have been reported on Medhub. XGC often mimics gallbladder cancer (GBC) and prompt diagnosis is critical due to significant complications including fistula formation, spread to pancreatic sources, or empyema’s, such as our case.
Case Description/Methods: A 64-year Caucasian male, with no past medical history, presented with painless jaundice and 50 lb unintentional weight loss over the past year. Strangely, he denied any abdominal pain, nausea or vomiting, but had high grade fevers. Labs showed total bilirubin of 15.3 mg/dl, direct bilirubin of 8.2 mg/dl, and elevated CA19-9 >7000. CT of the Abdomen & MRCP showed diffuse GB wall thickening with fat stranding but no CBD dilation. The initial working diagnosis was GBC based on imaging findings, weight loss, and elevated CA 19-9. Further work up with EUS, ERCP, ruling out intrinsic liver pathology with a negative liver biopsy, and having Klebsiella & Morganella bacteremia all pointed towards cholecystitis. Due to the worsening jaundice, ERCP with CBD stent and IR guided cholecystostomy tube were placed with improvement of his labs. Eventual high-risk cholecystectomy was performed which confirmed severe GB empyema but no obvious mass. Surgical pathology confirmed XGC with abscess. He successfully completed his IV antibiotics Cefepime/Flagyl. 4 weeks later, his biliary stent and cholecystostomy tube were removed as outpatient with complete normalization of his LFTs.
Discussion: Our patient had an abnormal clinical presentation of XGC without classic biliary symptoms or leukocytosis. Often, the presentation is misleading due to mass like findings on imaging and falsely elevated bilirubin tumor markers. Due diligence to rule out GBC is required but often the diagnosis of XGC can only be made via surgical pathology.
According to the Tokyo Guidelines, our patient had moderate acute cholangitis based on fevers, hyperbilirubinemia, hypoalbuminemia, and cholelithiasis on imaging. Even though there was no CBD dilatation yet, the substantial evidence of biliary obstruction, fevers, bacteremia, and GB empyema clearly indicated early ascending cholangitis. It is imperative clinicians stay vigilant about XGC in diagnosis because prompt surgical planning could prevent worsening cholangitis and often mislabeled diagnosis of GBC.

Disclosures:
Michael Su, MD1, Allyson Pagan, MD2, Viraj Modi, BS, DO2, Ruchir Paladiya, MBBS3, Bhavtosh Dedania, MD4. P0127 - Diagnostic Dilemma of Gallbladder Cancer vs Rare Cholecystitis/Cholangitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1HCA West Florida, Brandon, FL; 2HCA West Florida Brandon, Brandon, FL; 3UConn Health, Hartford, CT; 4HCA Florida Brandon Hospital, Brandon, FL
Introduction: Xanthogranulomatous Cholecystitis (XGC) is a rare type of cholecystitis that poses a diagnostic challenge. Cholangitis is an even rarer complication as only 5 such cases of XGC with cholangitis have been reported on Medhub. XGC often mimics gallbladder cancer (GBC) and prompt diagnosis is critical due to significant complications including fistula formation, spread to pancreatic sources, or empyema’s, such as our case.
Case Description/Methods: A 64-year Caucasian male, with no past medical history, presented with painless jaundice and 50 lb unintentional weight loss over the past year. Strangely, he denied any abdominal pain, nausea or vomiting, but had high grade fevers. Labs showed total bilirubin of 15.3 mg/dl, direct bilirubin of 8.2 mg/dl, and elevated CA19-9 >7000. CT of the Abdomen & MRCP showed diffuse GB wall thickening with fat stranding but no CBD dilation. The initial working diagnosis was GBC based on imaging findings, weight loss, and elevated CA 19-9. Further work up with EUS, ERCP, ruling out intrinsic liver pathology with a negative liver biopsy, and having Klebsiella & Morganella bacteremia all pointed towards cholecystitis. Due to the worsening jaundice, ERCP with CBD stent and IR guided cholecystostomy tube were placed with improvement of his labs. Eventual high-risk cholecystectomy was performed which confirmed severe GB empyema but no obvious mass. Surgical pathology confirmed XGC with abscess. He successfully completed his IV antibiotics Cefepime/Flagyl. 4 weeks later, his biliary stent and cholecystostomy tube were removed as outpatient with complete normalization of his LFTs.
Discussion: Our patient had an abnormal clinical presentation of XGC without classic biliary symptoms or leukocytosis. Often, the presentation is misleading due to mass like findings on imaging and falsely elevated bilirubin tumor markers. Due diligence to rule out GBC is required but often the diagnosis of XGC can only be made via surgical pathology.
According to the Tokyo Guidelines, our patient had moderate acute cholangitis based on fevers, hyperbilirubinemia, hypoalbuminemia, and cholelithiasis on imaging. Even though there was no CBD dilatation yet, the substantial evidence of biliary obstruction, fevers, bacteremia, and GB empyema clearly indicated early ascending cholangitis. It is imperative clinicians stay vigilant about XGC in diagnosis because prompt surgical planning could prevent worsening cholangitis and often mislabeled diagnosis of GBC.

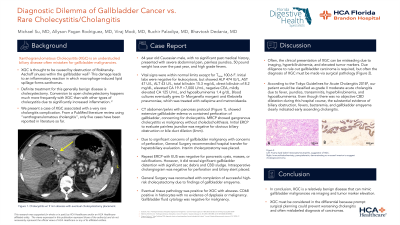
Figure: Figure 1.
Top: Foamy lipid laden histiocytes and neutrophils.
Bottom: Immunohistiochemistry, pancytokeratin, demonstrating no mucosal invasion to suggest cholangiocarcinoma.
Top: Foamy lipid laden histiocytes and neutrophils.
Bottom: Immunohistiochemistry, pancytokeratin, demonstrating no mucosal invasion to suggest cholangiocarcinoma.
Disclosures:
Michael Su indicated no relevant financial relationships.
Allyson Pagan indicated no relevant financial relationships.
Viraj Modi indicated no relevant financial relationships.
Ruchir Paladiya indicated no relevant financial relationships.
Bhavtosh Dedania indicated no relevant financial relationships.
Michael Su, MD1, Allyson Pagan, MD2, Viraj Modi, BS, DO2, Ruchir Paladiya, MBBS3, Bhavtosh Dedania, MD4. P0127 - Diagnostic Dilemma of Gallbladder Cancer vs Rare Cholecystitis/Cholangitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
