Sunday Poster Session
Category: Biliary/Pancreas
P0130 - Disconnected Duct Syndrome – A Rare Complication of Pancreatitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Frank L. Ventura, MD
Wake Forest Baptist Health
Winston-Salem, NC
Presenting Author(s)
Frank L. Ventura, MD, William Lippert, MD, MPH
Wake Forest Baptist Health, Winston-Salem, NC
Introduction: Disconnected Pancreatic Duct Syndrome (DPDS) is a rare complication of a common disease. Typically, DPDS occurs from necrotizing pancreatitis, chronic pancreatitis, abdominal surgery or trauma. Herein, we present a case of DPDS from non-necrotizing, acute pancreatitis.
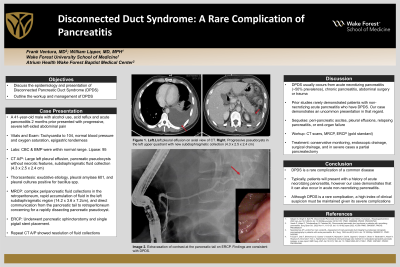
Case Description/Methods: A 41-year-old male with a history of alcohol use and acute pancreatitis (2 months prior) presented with progressive, severe left-sided abdominal pain that was worse with moving. He had no associated nausea, vomiting, diarrhea, shortness of breath, or back pain. Vitals were normal other than a heart rate of 104. Labs divulged a slightly elevated lipase of 95. Computed tomography (CTAP) demonstrated a large left-sided pleural effusion, non-necrotic pancreatic pseudocysts, and a subdiaphragmatic fluid collection (4.3 x 2.5 x 2.4 cm). A thoracentesis of the pleural effusion revealed an amylase of 601, exudative effusion, and cultures positive for bacillus species suggestive of pancreatic etiology. He was started on ciprofloxacin for 2 weeks.
A subsequent MRCP confirmed complex peripancreatic ascites, rapid subdiaphragmatic fluid accumulation (14.2 x 3.6 x 7.2cm), and a fistula from the pancreatic tail to retroperitoneum concerning for a rapidly dissecting pancreatic pseudocyst. He ultimately underwent an ERCP with pancreatic sphincterotomy and single pigtail stent placement. The subdiaphragmatic collection was deemed undrainable by interventional radiology. Symptoms rapidly improved and the patient was discharged. CT AP 1-week post-discharge showed a reduced size of subdiaphragmatic fluid collections (2.1 x 2.4 x 2.9 cm) consistent with resolution post-stent.
Discussion: DPDS is a rare complication of a common disease. Patients can present with a variety of sequelae depending on the fistula location, including peri-pancreatic ascites, pleural effusions, and relapsing pancreatitis. If left untreated, enzymatic autodigestion can lead to severe complications such as end-organ failure. Workup typically includes CT scans and MRCP and is ultimately confirmed via ERCP. Management may entail conservative monitoring, endoscopic drainage with ERCP, surgical drainage, or in severe cases a partial pancreatectomy may be performed.
Typically, patients will present with a history of necrotizing pancreatitis. Our case demonstrates that it can also occur in acute non-necrotizing pancreatitis. Although DPDS is a rare complication, a high index of clinical suspicion must be maintained given its severe complications.
Disclosures:
Frank L. Ventura, MD, William Lippert, MD, MPH. P0130 - Disconnected Duct Syndrome – A Rare Complication of Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Wake Forest Baptist Health, Winston-Salem, NC
Introduction: Disconnected Pancreatic Duct Syndrome (DPDS) is a rare complication of a common disease. Typically, DPDS occurs from necrotizing pancreatitis, chronic pancreatitis, abdominal surgery or trauma. Herein, we present a case of DPDS from non-necrotizing, acute pancreatitis.
Case Description/Methods: A 41-year-old male with a history of alcohol use and acute pancreatitis (2 months prior) presented with progressive, severe left-sided abdominal pain that was worse with moving. He had no associated nausea, vomiting, diarrhea, shortness of breath, or back pain. Vitals were normal other than a heart rate of 104. Labs divulged a slightly elevated lipase of 95. Computed tomography (CTAP) demonstrated a large left-sided pleural effusion, non-necrotic pancreatic pseudocysts, and a subdiaphragmatic fluid collection (4.3 x 2.5 x 2.4 cm). A thoracentesis of the pleural effusion revealed an amylase of 601, exudative effusion, and cultures positive for bacillus species suggestive of pancreatic etiology. He was started on ciprofloxacin for 2 weeks.
A subsequent MRCP confirmed complex peripancreatic ascites, rapid subdiaphragmatic fluid accumulation (14.2 x 3.6 x 7.2cm), and a fistula from the pancreatic tail to retroperitoneum concerning for a rapidly dissecting pancreatic pseudocyst. He ultimately underwent an ERCP with pancreatic sphincterotomy and single pigtail stent placement. The subdiaphragmatic collection was deemed undrainable by interventional radiology. Symptoms rapidly improved and the patient was discharged. CT AP 1-week post-discharge showed a reduced size of subdiaphragmatic fluid collections (2.1 x 2.4 x 2.9 cm) consistent with resolution post-stent.
Discussion: DPDS is a rare complication of a common disease. Patients can present with a variety of sequelae depending on the fistula location, including peri-pancreatic ascites, pleural effusions, and relapsing pancreatitis. If left untreated, enzymatic autodigestion can lead to severe complications such as end-organ failure. Workup typically includes CT scans and MRCP and is ultimately confirmed via ERCP. Management may entail conservative monitoring, endoscopic drainage with ERCP, surgical drainage, or in severe cases a partial pancreatectomy may be performed.
Typically, patients will present with a history of necrotizing pancreatitis. Our case demonstrates that it can also occur in acute non-necrotizing pancreatitis. Although DPDS is a rare complication, a high index of clinical suspicion must be maintained given its severe complications.
Disclosures:
Frank Ventura indicated no relevant financial relationships.
William Lippert indicated no relevant financial relationships.
Frank L. Ventura, MD, William Lippert, MD, MPH. P0130 - Disconnected Duct Syndrome – A Rare Complication of Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
