Sunday Poster Session
Category: Biliary/Pancreas
P0132 - Long-Standing Main Pancreatic Duct Intraductal Papillary Mucinous Neoplasm Treated With Double Papillae Endoscopic Sphincterotomy and Stent Placement
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Alp S. Kahveci, MD
University of Iowa Hospital & Clinics
Iowa City, Iowa
Presenting Author(s)
Alp S. Kahveci, MD1, George Win, BS2, Ahmed I.A. Swi, MD2, Faisal A.. Bukeirat, MD3
1University of Iowa Hospital & Clinics, Iowa City, IA; 2University of Missouri-Columbia, Columbia, MO; 3University of Missouri at Columbia, Columbia, MO
Introduction: First described in 1982 in Japan, intraductal papillary mucinous neoplasms (IPMN) represent cystic dilations of the main pancreatic duct (MD-IPMN) and/or branch ducts (BD-IPMN) that secrete thick mucin. Given their capacity for malignant transformation, early detection is critical. Here, we present a case of long-standing MD-IPMN treated with double papillae endoscopic sphincterotomy and stent placement.
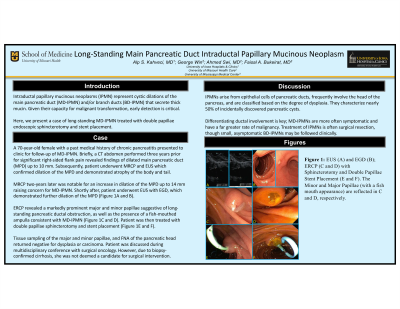
Case Description/Methods: A 70-year-old female with a past medical history of chronic pancreatitis presented to the gastroenterology clinic for follow-up of MD-IPMN. Briefly, a CT abdomen performed three years prior for significant right-sided flank pain revealed findings of dilated main pancreatic duct (MPD) up to 10 mm. Subsequently, patient underwent MRCP and EUS which confirmed dilation of the MPD and demonstrated atrophy of the body and tail. MRCP two-years later was notable for an increase in dilation of the MPD up to 14 mm raising concern for MD-IMPN. Shortly after, patient underwent EUS with EGD, which demonstrated further dilation of the MPD (Figure 1A and B). ERCP revealed a markedly prominent major and minor papillae suggestive of long-standing pancreatic ductal obstruction, as well as the presence of a fish-mouthed ampulla consistent with MD-IPMN (Figure 1C and D). Patient was then treated with double papillae sphincterotomy and stent placement (Figure 1E and F). Tissue sampling of the major and minor papillae, and FNA of the pancreatic head returned negative for dysplasia or carcinoma. Patient was discussed during multidisciplinary conference with surgical oncology. However, due to biopsy-confirmed cirrhosis, she was not deemed a candidate for surgical intervention.
Discussion: IPMNs arise from epithelial cells of pancreatic ducts, frequently involve the head of the pancreas, are classified based on the degree of dysplasia, and characterize nearly 50% of incidentally discovered pancreatic cysts. Under a quarter of patients may present with extra-pancreatic neoplasms. Differentiating ductal involvement is key; MD-IPMNs are more often symptomatic and have a far greater rate of malignancy. Treatment is often surgical resection, though small, asymptomatic BD-IPMNs may be followed clinically.

Disclosures:
Alp S. Kahveci, MD1, George Win, BS2, Ahmed I.A. Swi, MD2, Faisal A.. Bukeirat, MD3. P0132 - Long-Standing Main Pancreatic Duct Intraductal Papillary Mucinous Neoplasm Treated With Double Papillae Endoscopic Sphincterotomy and Stent Placement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Iowa Hospital & Clinics, Iowa City, IA; 2University of Missouri-Columbia, Columbia, MO; 3University of Missouri at Columbia, Columbia, MO
Introduction: First described in 1982 in Japan, intraductal papillary mucinous neoplasms (IPMN) represent cystic dilations of the main pancreatic duct (MD-IPMN) and/or branch ducts (BD-IPMN) that secrete thick mucin. Given their capacity for malignant transformation, early detection is critical. Here, we present a case of long-standing MD-IPMN treated with double papillae endoscopic sphincterotomy and stent placement.
Case Description/Methods: A 70-year-old female with a past medical history of chronic pancreatitis presented to the gastroenterology clinic for follow-up of MD-IPMN. Briefly, a CT abdomen performed three years prior for significant right-sided flank pain revealed findings of dilated main pancreatic duct (MPD) up to 10 mm. Subsequently, patient underwent MRCP and EUS which confirmed dilation of the MPD and demonstrated atrophy of the body and tail. MRCP two-years later was notable for an increase in dilation of the MPD up to 14 mm raising concern for MD-IMPN. Shortly after, patient underwent EUS with EGD, which demonstrated further dilation of the MPD (Figure 1A and B). ERCP revealed a markedly prominent major and minor papillae suggestive of long-standing pancreatic ductal obstruction, as well as the presence of a fish-mouthed ampulla consistent with MD-IPMN (Figure 1C and D). Patient was then treated with double papillae sphincterotomy and stent placement (Figure 1E and F). Tissue sampling of the major and minor papillae, and FNA of the pancreatic head returned negative for dysplasia or carcinoma. Patient was discussed during multidisciplinary conference with surgical oncology. However, due to biopsy-confirmed cirrhosis, she was not deemed a candidate for surgical intervention.
Discussion: IPMNs arise from epithelial cells of pancreatic ducts, frequently involve the head of the pancreas, are classified based on the degree of dysplasia, and characterize nearly 50% of incidentally discovered pancreatic cysts. Under a quarter of patients may present with extra-pancreatic neoplasms. Differentiating ductal involvement is key; MD-IPMNs are more often symptomatic and have a far greater rate of malignancy. Treatment is often surgical resection, though small, asymptomatic BD-IPMNs may be followed clinically.

Figure: Figure 1: EUS (A) and EGD (B); ERCP (C and D) with Sphincterotomy and Double Papillae Stent Placement (E and F)
Disclosures:
Alp Kahveci: Arbutus Biopharma Corp – Stock-publicly held company(excluding mutual/index funds). Bionano Genomics Inc – Stock-publicly held company(excluding mutual/index funds). Biontech SE – Stock-publicly held company(excluding mutual/index funds). Moderna Inc – Stock-publicly held company(excluding mutual/index funds). Pfizer Inc – Stock-publicly held company(excluding mutual/index funds). Senseonics Holdings Inc – Stock-publicly held company(excluding mutual/index funds).
George Win indicated no relevant financial relationships.
Ahmed Swi indicated no relevant financial relationships.
Faisal Bukeirat indicated no relevant financial relationships.
Alp S. Kahveci, MD1, George Win, BS2, Ahmed I.A. Swi, MD2, Faisal A.. Bukeirat, MD3. P0132 - Long-Standing Main Pancreatic Duct Intraductal Papillary Mucinous Neoplasm Treated With Double Papillae Endoscopic Sphincterotomy and Stent Placement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
