Sunday Poster Session
Category: Biliary/Pancreas
P0135 - A Case of Necrotizing Pancreatitis After IR Embolization for the Management of Acute Upper GI Bleed
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Lindsey Donnelly, MD, MS
John T. Mather Memorial Hospital at Northwell Health
Rocky Point, NY
Presenting Author(s)
Lindsey Donnelly, MD, MS1, David Kadosh, MD2, Glen Granati, MD2
1John T. Mather Memorial Hospital at Northwell Health, Rocky Point, NY; 2John T. Mather Memorial Hospital at Northwell Health, Port Jefferson, NY
Introduction: Transarterial embolization (TAE) is commonly performed for cases of recurrent gastrointestinal (GI) bleeding after endoscopic management or cases that are not amenable to endoscopic treatment. Adverse events associated with IR embolization are those associated with arteriography, ischemia and infarction. Acute pancreatitis is a rare complication of embolization and very few cases of necrotizing pancreatitis have been reported. This case report presents a patient who suffered acute necrotizing pancreatitis after TAE for the management of an acute upper GI bleed.
Case Description/Methods: 52-year-old male with history of SLE on steroids, alcohol abuse and pancreatic pseudocyst presented with an acute upper GI bleed with hemodynamic instability requiring massive transfusion protocol and intubation for airway protection. CT angiogram showed angiodysplasia of the transverse duodenum with active extravasation. Endoscopic intervention was deferred due to hemodynamic instability and the patient underwent mesenteric angiogram with IR guided gastroduodenal artery embolization with the coil extending into the inferior duodenal arcade branch which communicated with a branch of the inferior pancreaticoduodenal artery. The bleeding resolved completely after embolization. The patient was extubated and 4 days later had complaints of severe epigastric abdominal pain. CT abdomen showed acute necrotizing pancreatitis involving the pancreatic body. The patient’s hospital course was complicated by acute respiratory distress syndrome (ARDS) which was attributed to pancreatitis, requiring reintubation.
Discussion: Some cases of acute GI bleeding require rapid TAE in order to control bleeding when endoscopic management may not be possible or may worsen the patient’s hemodynamic status. As with most procedures, embolization has complications. Ischemia and infarction are known complications of the procedure but with the vast collateral system of the gastrointestinal tract, are relatively uncommon. The pancreas is supplied by the splenic, gastroduodenal and superior mesenteric arteries however, in cases where the blood supply may have been previously compromised such as in cases of previous pancreatitis or pseudocysts, this complication may be more common. In our patient, who had a history of alcohol abuse and likely previous cases of pancreatitis given his known pseudocyst, we propose that his collateral blood supply may have been previously compromised leading to this acute complication.

Disclosures:
Lindsey Donnelly, MD, MS1, David Kadosh, MD2, Glen Granati, MD2. P0135 - A Case of Necrotizing Pancreatitis After IR Embolization for the Management of Acute Upper GI Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1John T. Mather Memorial Hospital at Northwell Health, Rocky Point, NY; 2John T. Mather Memorial Hospital at Northwell Health, Port Jefferson, NY
Introduction: Transarterial embolization (TAE) is commonly performed for cases of recurrent gastrointestinal (GI) bleeding after endoscopic management or cases that are not amenable to endoscopic treatment. Adverse events associated with IR embolization are those associated with arteriography, ischemia and infarction. Acute pancreatitis is a rare complication of embolization and very few cases of necrotizing pancreatitis have been reported. This case report presents a patient who suffered acute necrotizing pancreatitis after TAE for the management of an acute upper GI bleed.
Case Description/Methods: 52-year-old male with history of SLE on steroids, alcohol abuse and pancreatic pseudocyst presented with an acute upper GI bleed with hemodynamic instability requiring massive transfusion protocol and intubation for airway protection. CT angiogram showed angiodysplasia of the transverse duodenum with active extravasation. Endoscopic intervention was deferred due to hemodynamic instability and the patient underwent mesenteric angiogram with IR guided gastroduodenal artery embolization with the coil extending into the inferior duodenal arcade branch which communicated with a branch of the inferior pancreaticoduodenal artery. The bleeding resolved completely after embolization. The patient was extubated and 4 days later had complaints of severe epigastric abdominal pain. CT abdomen showed acute necrotizing pancreatitis involving the pancreatic body. The patient’s hospital course was complicated by acute respiratory distress syndrome (ARDS) which was attributed to pancreatitis, requiring reintubation.
Discussion: Some cases of acute GI bleeding require rapid TAE in order to control bleeding when endoscopic management may not be possible or may worsen the patient’s hemodynamic status. As with most procedures, embolization has complications. Ischemia and infarction are known complications of the procedure but with the vast collateral system of the gastrointestinal tract, are relatively uncommon. The pancreas is supplied by the splenic, gastroduodenal and superior mesenteric arteries however, in cases where the blood supply may have been previously compromised such as in cases of previous pancreatitis or pseudocysts, this complication may be more common. In our patient, who had a history of alcohol abuse and likely previous cases of pancreatitis given his known pseudocyst, we propose that his collateral blood supply may have been previously compromised leading to this acute complication.

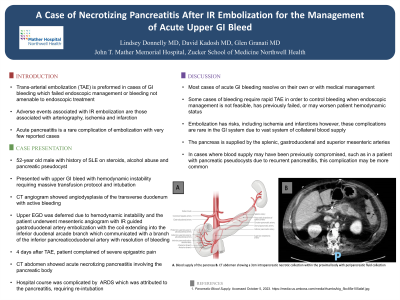
Figure: CT abdomen showing a 3cm intrapancreatic necrotic collection within the proximal body with peripancreatic fluid collection
Disclosures:
Lindsey Donnelly indicated no relevant financial relationships.
David Kadosh indicated no relevant financial relationships.
Glen Granati indicated no relevant financial relationships.
Lindsey Donnelly, MD, MS1, David Kadosh, MD2, Glen Granati, MD2. P0135 - A Case of Necrotizing Pancreatitis After IR Embolization for the Management of Acute Upper GI Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
