Sunday Poster Session
Category: Biliary/Pancreas
P0136 - A Case of Sevelamer Deposition and Subsequent Proctitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Thomas R. Checketts, DO
Creighton University School of Medicine
Omaha, NE
Presenting Author(s)
Thomas Checketts, DO1, Mohammed Qasswal, MD2, Joyce Pazhayattil, MBBS2, Clay Jarrell, MD2, Robert T.. Kizer, MD1
1Creighton University School of Medicine, Omaha, NE; 2Creighton University, Omaha, NE
Introduction: Phosphate control is an important consideration in chronic kidney disease to maintain bone health. The Kidney Disease Improving Global Outcomes (KDIGO) 2017 guidelines recommend that it be given to patients with persistent hyperphosphatemia regardless of whether they are receiving dialysis or not. Phosphate is controlled through dietary reduction, phosphate binders, calcium supplements, and/or native Vitamin D intake. In patients with ESRD, phosphate control is a challenge to manage. Two large studies estimated only 53-75% of patients are being adequately controlled. One uncommon complication of sevelamer is recto-sigmoid ulcerations. There are documented cases in both adult and pediatric patients.
Case Description/Methods: This is a case of a 60-year-old black female who presented with supratherapeutic international normalized ratio (INR) and gastrointestinal (GI) bleed. Past medical history included atrial fibrillation on chronic anticoagulation and type 2 diabetes mellitus. She was hemodialysis dependent due to a failed kidney transplant. She presented with abnormal labs and an INR of 7 detected at dialysis. In the months prior, she had been admitted to other hospitals for hemorrhagic shock due secondary to ischemic colitis. Computed tomography (CT) scans showed subcentimeter mesorectal lymph nodes suspicious for proctitis.
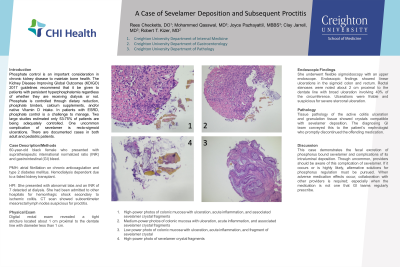
Digital rectal exam revealed a tight stricture located about 1 cm proximal to the dentate line with diameter less than 1 cm. She underwent flexible sigmoidoscopy with an upper endoscope. Endoscopic findings showed linear ulcerations in the sigmoid colon and rectum. Rectal stenoses were noted about 2 cm proximal to the dentate line with broad ulceration involving 40% of the circumference. Ulcerations were friable and suspicious for severe stercoral ulceration.
Tissue pathology of the active colitis ulceration and granulation tissue showed crystals compatible with sevelamer deposition. The diagnosing GI team conveyed this to the patient’s nephrologist who promptly discontinued the offending medication.
Discussion: This case demonstrates the fecal excretion of phosphorus bound sevelamer and complications of its intraluminal deposition. Though uncommon, providers should be aware of this complication of sevelamer. If it occurs or is highly likely, alternative solutions for phosphorus regulation must be pursued. When adverse medication effects occur, collaboration with other providers is required; especially when the medication is not one that GI teams regularly prescribe.

Disclosures:
Thomas Checketts, DO1, Mohammed Qasswal, MD2, Joyce Pazhayattil, MBBS2, Clay Jarrell, MD2, Robert T.. Kizer, MD1. P0136 - A Case of Sevelamer Deposition and Subsequent Proctitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Creighton University School of Medicine, Omaha, NE; 2Creighton University, Omaha, NE
Introduction: Phosphate control is an important consideration in chronic kidney disease to maintain bone health. The Kidney Disease Improving Global Outcomes (KDIGO) 2017 guidelines recommend that it be given to patients with persistent hyperphosphatemia regardless of whether they are receiving dialysis or not. Phosphate is controlled through dietary reduction, phosphate binders, calcium supplements, and/or native Vitamin D intake. In patients with ESRD, phosphate control is a challenge to manage. Two large studies estimated only 53-75% of patients are being adequately controlled. One uncommon complication of sevelamer is recto-sigmoid ulcerations. There are documented cases in both adult and pediatric patients.
Case Description/Methods: This is a case of a 60-year-old black female who presented with supratherapeutic international normalized ratio (INR) and gastrointestinal (GI) bleed. Past medical history included atrial fibrillation on chronic anticoagulation and type 2 diabetes mellitus. She was hemodialysis dependent due to a failed kidney transplant. She presented with abnormal labs and an INR of 7 detected at dialysis. In the months prior, she had been admitted to other hospitals for hemorrhagic shock due secondary to ischemic colitis. Computed tomography (CT) scans showed subcentimeter mesorectal lymph nodes suspicious for proctitis.
Digital rectal exam revealed a tight stricture located about 1 cm proximal to the dentate line with diameter less than 1 cm. She underwent flexible sigmoidoscopy with an upper endoscope. Endoscopic findings showed linear ulcerations in the sigmoid colon and rectum. Rectal stenoses were noted about 2 cm proximal to the dentate line with broad ulceration involving 40% of the circumference. Ulcerations were friable and suspicious for severe stercoral ulceration.
Tissue pathology of the active colitis ulceration and granulation tissue showed crystals compatible with sevelamer deposition. The diagnosing GI team conveyed this to the patient’s nephrologist who promptly discontinued the offending medication.
Discussion: This case demonstrates the fecal excretion of phosphorus bound sevelamer and complications of its intraluminal deposition. Though uncommon, providers should be aware of this complication of sevelamer. If it occurs or is highly likely, alternative solutions for phosphorus regulation must be pursued. When adverse medication effects occur, collaboration with other providers is required; especially when the medication is not one that GI teams regularly prescribe.

Figure: 1 High-power photos of colonic mucosa with ulceration, acute inflammation, and associated sevelamer crystal fragments
2 Medium-power photos of colonic mucosa with ulceration, acute inflammation, and associated sevelamer crystal fragments
3 Low power photo of colonic mucosa with ulceration, acute inflammation, and fragment of sevelamer crystal
4 High-power photo of sevelamer crystal fragments
2 Medium-power photos of colonic mucosa with ulceration, acute inflammation, and associated sevelamer crystal fragments
3 Low power photo of colonic mucosa with ulceration, acute inflammation, and fragment of sevelamer crystal
4 High-power photo of sevelamer crystal fragments
Disclosures:
Thomas Checketts indicated no relevant financial relationships.
Mohammed Qasswal indicated no relevant financial relationships.
Joyce Pazhayattil indicated no relevant financial relationships.
Clay Jarrell indicated no relevant financial relationships.
Robert Kizer indicated no relevant financial relationships.
Thomas Checketts, DO1, Mohammed Qasswal, MD2, Joyce Pazhayattil, MBBS2, Clay Jarrell, MD2, Robert T.. Kizer, MD1. P0136 - A Case of Sevelamer Deposition and Subsequent Proctitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
